
Trying to figure out why you feel off after starting Alna is a combined oral contraceptive pill that blends levonorgestrel and ethinyl estradiol to prevent pregnancy? You’re not alone. Many users notice a handful of bodily signals that can feel confusing or even alarming. The good news is that most of these reactions are predictable, manageable, and often fade as your body adjusts.
What’s Inside Alna? The Core Ingredients
- Levonorgestrel is a synthetic progestogen that thickens cervical mucus and stops ovulation.
- Ethinyl estradiol is a synthetic estrogen that stabilizes the uterine lining and helps regulate the menstrual cycle.
Because Alna packs both hormones, it falls under the broader category of hormonal contraceptive any medication that uses synthetic hormones to prevent pregnancy. Knowing the two active agents lets you anticipate what your body might protest.
Common Side Effects and Why They happen
Most people experience at least one of the following within the first few months:
| Side effect | Why it occurs |
|---|---|
| Nausea a stomach upset feeling | Estrogen can slow gastric motility, while progesterone relaxes smooth muscle. |
| Headache painful pressure in the head | Fluctuations in estrogen influence blood vessel tone. |
| Breast tenderness soreness or swelling in the breasts | Both hormones stimulate breast tissue growth. |
| Mood changes irritability, anxiety, or low mood | Neurochemical shifts caused by hormone levels can affect serotonin. |
| Weight fluctuation | Water retention from estrogen and appetite changes from progesterone. |
| Spotting between periods | Initial endometrial instability as the lining adapts. |
Most of these fade after 2‑3 cycles. However, if any symptom feels severe, it’s worth a chat with your healthcare provider.
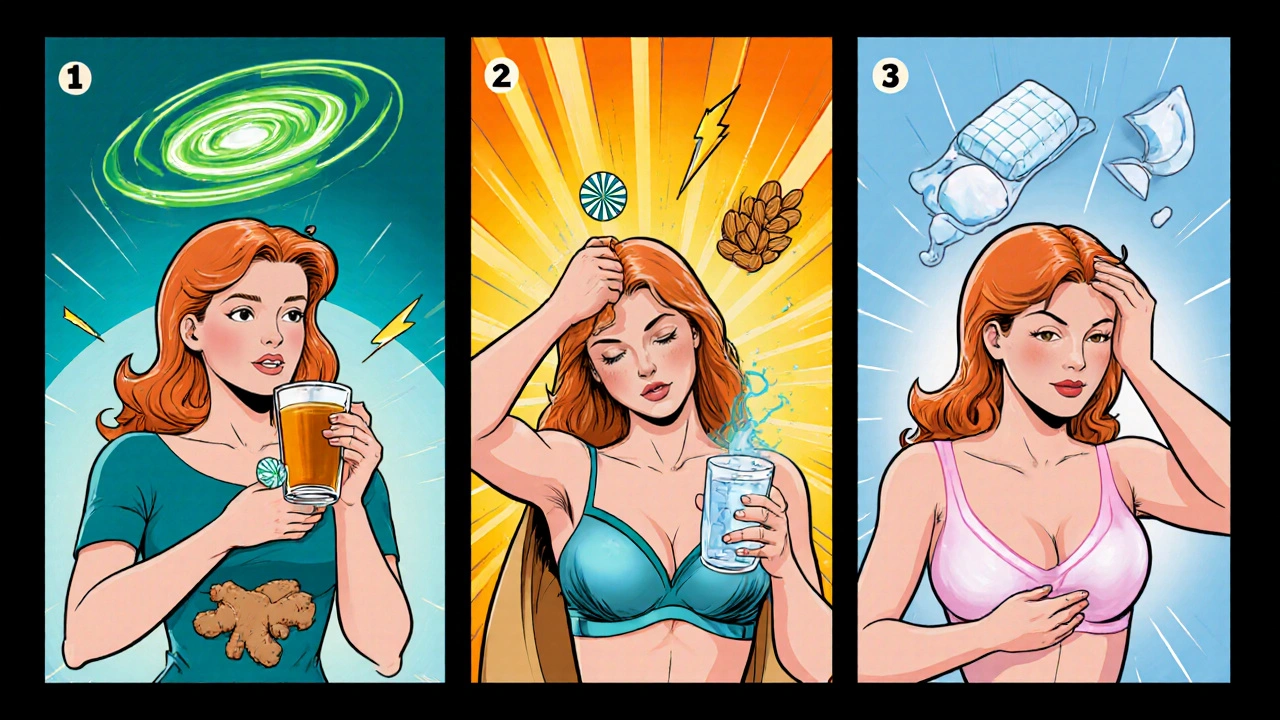
How to Tackle Each Symptom
- Nausea
- Take the pill with food or right before bedtime.
- Stay hydrated; sip ginger tea or suck on peppermint lozenges.
- If vomiting occurs within two hours of dosing, retake a missed tablet and consider a backup method for 48hours.
- Headache
- Maintain a regular sleep schedule; erratic sleep worsens vascular headaches.
- Magnesium‑rich snacks (almonds, spinach) can reduce intensity.
- Over‑the‑counter ibuprofen works for most, but avoid aspirin if you have a bleeding disorder.
- Breast tenderness
- Wear a supportive bra, especially during the first weeks.
- Cool compresses for 10‑15minutes help soothe swelling.
- If pain worsens after the second month, check with a clinician for other causes.
- Mood changes
- Track emotions in a journal; pattern‑recognition often reveals triggers.
- Regular aerobic activity (30minutes, three times a week) stabilizes serotonin.
- If depression persists beyond six weeks, discuss alternative formulations.
- Weight changes
- Focus on whole foods and limit sodium to curb water retention.
- Strength training helps preserve lean mass.
- Spotting
- Take the pill at the same time daily; missed doses can cause hormonal swings.
- Use a panty liner if spotting is light; heavy bleeding warrants a doctor’s look.
When to Seek Professional Help
Most side effects are harmless, but a few red flags demand immediate attention:
- Severe abdominal pain combined with dizziness - could signal a blood clot.
- Sudden vision changes or headache that doesn’t improve with OTC meds - possible hypertension.
- Persistent vomiting for more than 24hours - risk of dehydration and missed dose.
- Signs of allergic reaction (hives, swelling of lips or throat) - stop the pill and call emergency services.
Your healthcare provider the doctor, nurse practitioner, or pharmacist who prescribed the medication can assess whether you need a dosage tweak, a switch to a different formulation, or a non‑hormonal alternative.
Drug Interactions to Watch
Alna’s effectiveness can drop if you’re taking certain medicines. Keep an eye on:
- Antibiotics like rifampin - they increase liver enzymes that break down hormones.
- Anticonvulsants (e.g., carbamazepine, phenytoin) - similar enzyme‑inducing effect.
- St.John’s wort - a herbal supplement that can halve contraceptive reliability.
- Antiretrovirals used for HIV - some protease inhibitors may boost hormone levels, causing more side effects.
If you start any new medication, ask your provider whether you need a backup condom for the next month.
Key Takeaways
- Alna combines levonorgestrel and ethinyl estradiol, so most side effects stem from hormonal shifts.
- Typical reactions include nausea, headache, breast tenderness, mood swings, weight changes, and spotting.
- Most symptoms ease after 2‑3 cycles; simple tricks like taking the pill with food or using a supportive bra can help.
- Seek urgent care for severe abdominal pain, vision changes, persistent vomiting, or allergic reactions.
- Always check for drug interactions; certain antibiotics, anticonvulsants, and herbal supplements can reduce effectiveness.
Frequently Asked Questions
How long do Alna side effects usually last?
Most users notice improvement after 2‑3 menstrual cycles. If a symptom persists beyond three months, talk to your clinician about switching formulations.
Can I take Alna if I’m on antibiotics?
Only a few antibiotics (like rifampin) affect Alna’s efficacy. Common courses such as amoxicillin or doxycycline are safe. Always confirm with your provider.
Is it normal to gain weight on Alna?
A small amount of water‑weight gain (1‑2lb) is common during the first month. Long‑term weight gain isn’t typical; lifestyle habits play a bigger role.
What should I do if I miss a pill?
Take the missed tablet as soon as you remember, then continue with the regular schedule. If you’re more than 24hours late, use a backup method (condom) for the next 7 days.
Can I switch from Alna to a non‑hormonal method?
Yes. Your provider can guide you through a transition plan, often using a barrier method for a month while your body clears the hormones.
Joy Luca
October 6, 2025 AT 02:25Yo, Alna’s pharmacodynamics hinge on synthetic progestogenic agonism and estrogenic receptor modulation which can precipitate gastrointestinal dysmotility and vasodilatory headache phenotypes. Grab a high‑fiber snack and hydrate like you’re in a desert marathon. Take the pill with a solid breakfast to blunt nausea spikes. Consistency in dosing time is the linchpin for endocrine stabilization.
Jessica Martins
October 7, 2025 AT 06:11The recommendations in the article are clinically sound; taking Alna with food, ensuring adequate magnesium intake, and monitoring for breakthrough bleeding align with standard practice. It is important to document any persistent symptoms and discuss them with a healthcare provider.
Doug Farley
October 8, 2025 AT 09:58Oh great, another miracle pill that makes you feel like you’re on a roller‑coaster of hormones. Nausea? Headache? Congratulations, you’ve earned the full side‑effect package. If you’re looking for a free ticket to “mood swing city,” Alna’s got a first‑class seat reserved.
Jeremy Olson
October 9, 2025 AT 13:45Thank you for sharing this comprehensive overview. The step‑by‑step management strategies, such as using ginger tea for nausea or supportive bras for breast tenderness, are practical and evidence‑based. Patients often appreciate clear guidance that can be integrated into daily routines.
Ada Lusardi
October 10, 2025 AT 17:31💊✨ Alna can be a wild ride but you’ve got this! 🌈 Keep a peppermint lozenge handy for queasy mornings 😌 and don’t forget those cozy bras for tender tummies 🩱💖 Remember, a little self‑care goes a long way 🌟
Pam Mickelson
October 11, 2025 AT 21:18Hey, nice rundown! I totally agree-taking the pill with breakfast and staying hydrated makes a huge difference. If you’re feeling off, just give your body a week or two and the symptoms usually chill out.
Joe V
October 13, 2025 AT 01:05Well, well, if it isn’t the “everything‑you‑need‑to‑know” guide. Kudos for the thoroughness, though I’d suggest a dash of caution when recommending magnesium to folks with kidney issues. Remember, one size does not fit all.
Scott Davis
October 14, 2025 AT 04:51Sounds solid. Keep the timing consistent.
Calvin Smith
October 15, 2025 AT 08:38Ah, the Alna saga-like a tropical storm of hormones that decides to crash your calm. If you wanted drama, you could've just binge‑watched a soap opera. Instead, you get spotting that makes you wonder if you’re secretly a vampire. Grab a drama‑free contraceptive if you’re over the theatrical side effects.
Brenda Hampton
October 16, 2025 AT 12:25Sticking to a routine with Alna can really smooth out those initial bumps. Tracking your symptoms each cycle helps you see patterns and empowers you to make informed adjustments with your provider.
Lara A.
October 17, 2025 AT 16:11Listen, folks, the pharmaceutical giants - yes, those shadowy conglomerates - have been hiding the true risks of hormonal pills for decades, and this article is just the tip of the iceberg, - so read the fine print, question the “standard” recommendations, - and never trust a single source without doing your own deep dive.
Oscar Brown
October 18, 2025 AT 19:58The discourse surrounding combined oral contraceptives such as Alna warrants a meticulous examination that transcends superficial anecdote.
One must first acknowledge the intricate biochemical cascade precipitated by levonorgestrel and ethinyl estradiol, each interacting with distinct nuclear receptors to orchestrate ovulatory suppression.
The resultant modulation of the hypothalamic‑pituitary‑gonadal axis manifests clinically in a spectrum of physiologic perturbations, ranging from gastro‑intestinal dyspepsia to vascular endothelial alterations.
It is incumbent upon the prescriber to elucidate these mechanistic underpinnings to the patient, thereby fostering an environment of informed consent.
Moreover, the temporal latency of side‑effect amelioration, typically spanning two to three menstrual cycles, should be contextualized within the broader pharmacokinetic half‑life of the constituent hormones.
Empirical evidence further suggests that concomitant administration of magnesium‑rich comestibles may attenuate cephalic discomfort via antagonism of calcium‑mediated vasoconstriction.
Nevertheless, such dietary adjuncts must be calibrated against the patient’s renal function to avert iatrogenic hypermagnesemia.
In addition, the potential for drug‑drug interactions, particularly with enzyme‑inducing agents such as rifampin or certain antiepileptics, mandates vigilant therapeutic monitoring.
Failure to account for these interactions may precipitate suboptimal contraceptive efficacy, an outcome antithetical to the overarching goal of reproductive autonomy.
The clinical practitioner should therefore maintain a comprehensive medication reconciliation at each encounter.
From an ethical perspective, the duty to disclose both common and rare adverse events aligns with the principle of non‑maleficence.
It is also prudent to consider alternative modalities, such as non‑hormonal barrier methods, should the patient’s risk‑benefit analysis deem them more suitable.
In summation, the interplay between pharmacodynamics, patient adherence, and systemic health variables constitutes a multifaceted tableau demanding scholarly diligence.
By integrating evidence‑based guidelines with individualized patient narratives, clinicians can navigate this complexity with prudence.
Ultimately, the aspiration is to empower the patient through transparent communication, thereby mitigating anxiety and enhancing therapeutic compliance.
Tommy Mains
October 19, 2025 AT 23:45Great summary! To add, keep a simple side‑effect diary-note the day, symptom, and any possible triggers. This record makes the follow‑up conversation with your provider more productive.