
Personalized Dry Mouth Oral Care Planner
Your Dry Mouth Situation
Living with dry mouth (xerostomia) can turn everyday tasks like eating, speaking, and smiling into uncomfortable chores. The good news? You can build an oral‑care routine that soothes the feeling, protects teeth, and keeps your mouth feeling fresh-all without relying on heavy‑duty products that worsen dryness.
What Exactly Is Dry Mouth?
Dry mouth is a condition where the salivary glands don’t produce enough saliva to keep the mouth moist. It isn’t just a nuisance; saliva plays a critical role in neutralising acids, washing away food particles, and fighting bacteria. When saliva drops, plaque builds faster, cavities rise, and the risk of gum disease climbs.
Common triggers include certain medications (antihistamines, antidepressants), medical conditions (diabetes, Sjögren’s syndrome), and lifestyle factors such as smoking or excessive caffeine.
Three Pillars of a Dry‑Mouth Friendly Routine
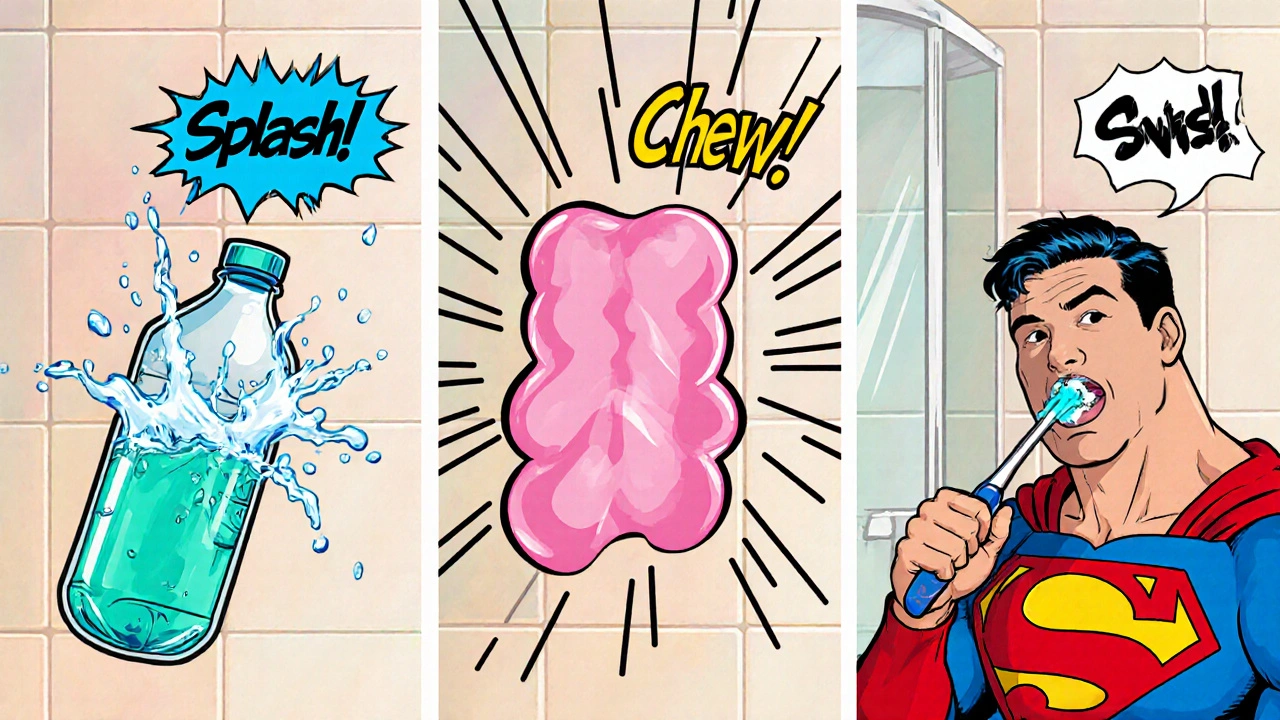
Think of the routine as a three‑part framework: hydrate, stimulate, and protect.
- Hydrate - Keep your body’s water balance in check.
- Stimulate Saliva - Use foods, gums, or devices that encourage natural flow.
- Protect Teeth and Gums - Choose gentle cleaning tools and moisture‑rich rinses.
Each pillar stacks on the next, creating a routine that works even on the toughest days.
Selecting a Toothbrush and Toothpaste That Won’t Irritate
Most people underestimate how much a toothbrush can affect dryness. A soft‑bristled brush is key; it cleans without scraping the already thin mucosal layer.
Toothbrush should have ultra‑soft (size 0) or extra‑soft bristles, a small head, and an ergonomic handle to keep pressure low. Pair it with a fluoride toothpaste that’s alcohol‑free and contains moisturising agents such as sorbitol or xylitol.
Why fluoride? It strengthens enamel, and a fluoride‑rich paste lowers the chance of cavities caused by the acid‑producing bacteria that thrive when saliva is scarce.
Mouthwash Options: Alcohol‑Free vs. Alcohol‑Based
Many over‑the‑counter rinses contain alcohol, which can evaporate moisture and leave a burning sensation. For dry‑mouth sufferers, an alcohol‑free mouthwash is the safer bet.
| Feature | Alcohol‑Free | Alcohol‑Based |
|---|---|---|
| Moisture Impact | Adds moisture, gentle on tissues | Dries out oral mucosa |
| Flavor | Mild, often mint or herbal | Strong, sometimes burning |
| Antimicrobial Power | Contains cetylpyridinium chloride or chlorhexidine (low concentration) | Usually contains ethanol‑based antiseptics |
| Best For | Dry mouth, sensitive gums, post‑radiation patients | General freshening, occasional use |
Choose a mouthwash with xylitol or glycerin - both act as humectants, pulling water into the oral cavity.
Boosting Saliva Production Naturally
While you can’t replace saliva entirely with a product, you can coax the glands to work harder.
- Sugar‑free gum - Chewing stimulates the parotid glands. Look for gum sweetened with xylitol; it also fights cavities.
- Hard, sugar‑free lozenges (often labelled “saliva‑stimulating”).
- Foods high in water content - cucumbers, watermelon, apples.
- Probiotic‑rich products like kefir or unsweetened yogurt, which may help maintain a balanced oral microbiome.
Even a few minutes of chewing after meals can boost flow by 50%.
Dietary and Lifestyle Hacks
What you put in your mouth matters just as much as what you brush away.
- Stay Hydrated: Aim for at least 2liters of water per day. Sip regularly, not just when thirsty.
- Limit caffeine and alcohol - both are diuretics that thin saliva.
- Avoid mouth‑drying foods like salty crackers or overly spicy dishes.
- Quit smoking; nicotine reduces salivary output and irritates tissues.
Small changes add up. Swapping a soda for water at lunch can preserve that thin layer of protection throughout the afternoon.

When to Call in a Professional
If you notice persistent sores, bad breath that won’t improve, or a sudden increase in cavities, it’s time to seek help.
Dental professional visits can include:
- Saliva‑flow tests (sialometry) to quantify the problem.
- Prescription‑strength saliva substitutes or stimulants.
- Medication review - sometimes a simple switch eliminates dry‑mouth side effects.
Regular cleanings (every six months) also let the dentist spot early decay before it becomes painful.
Quick Dry‑Mouth‑Friendly Oral Care Checklist
- Drink water in small sips throughout the day.
- Use a soft‑bristled toothbrush with fluoride, alcohol‑free toothpaste.
- Rinse with an alcohol‑free, xylitol‑based mouthwash twice daily.
- Chew xylitol gum or suck on a saliva‑stimulating lozenge after meals.
- Eat water‑rich fruits and vegetables; limit caffeine, alcohol, and salty snacks.
- Visit your dentist for a check‑up and discuss any medication‑induced dryness.
Follow these steps every morning and night, and you’ll notice less burning, fewer cavities, and a more comfortable smile.
Frequently Asked Questions
Can I use over‑the‑counter saliva substitutes?
Yes. Look for products that list glycerin, carboxymethylcellulose, or hydroxyethylcellulose as active ingredients. They coat the mouth and give a temporary feeling of moisture, but they don’t replace the protective enzymes in real saliva, so keep them as a supplement, not a replacement.
Is drinking water enough to cure dry mouth?
Hydration is essential but not sufficient. Water helps keep the mouth wet temporarily, but you still need saliva‑stimulating habits and protective products to maintain oral health long‑term.
Are there any toothpaste ingredients I should avoid?
Avoid toothpaste with sodium lauryl sulfate (SLS) if you have a sensitive mouth; SLS can increase irritation. Choose SLS‑free formulas that still contain fluoride.
How often should I replace my toothbrush?
Every three months, or sooner if the bristles become frayed. A worn brush can damage the delicate oral tissues you’re trying to protect.
Can certain medical conditions cause permanent dry mouth?
Conditions like Sjögren’s syndrome or radiation therapy to the head‑neck area can lead to lasting reduced salivary flow. Management focuses on symptom relief and rigorous oral‑care routines.
Jacob Hamblin
September 28, 2025 AT 15:37Staying hydrated first thing in the morning really helps my dry mouth.
Herman Rochelle
October 7, 2025 AT 21:50Make sure you sip water throughout the day, especially after any coffee or tea; a steady flow keeps the oral tissues moist and reduces that gritty feeling.
Stanley Platt
October 17, 2025 AT 04:04One might observe that employing an ultra‑soft brush, coupled with a fluoride toothpaste devoid of alcohol, significantly mitigates irritation; moreover, an alcohol‑free rinse enriched with glycerin serves as an excellent adjunct. 😊
Alice Settineri
October 26, 2025 AT 09:17Yo, if you’re chugging soda all day, no wonder your mouth feels like the Sahara-swap that junk for water or herbal tea and watch the desert melt away, pronto!
Dawson Turcott
November 4, 2025 AT 15:30Oh great, another “miracle” routine…yeah, chewing sugar‑free gum works, but only if you actually chewin’ it, not just stashin’ it in your pocket. 😏
Alex Jhonson
November 13, 2025 AT 21:44i found that even a tiny typo in my water‑intake log made me double‑check, but the routine itself-soft brush, fluoride paste, moisturizin’ rinse-still works fine.
Katheryn Cochrane
November 23, 2025 AT 03:57The prescribed plan reads like a corporate wellness brochure, all buzz‑words and no real nuance. While the suggestion to drink eight glasses a day is universally praised, it ignores individual metabolic variance and the impact of antihistamines that are notorious for xerostomia. Moreover, the recommendation to avoid caffeine and alcohol is overly simplistic; a moderate coffee habit can be accommodated with timed sips and saliva substitutes. The routine’s emphasis on ultra‑soft brushes is valid, yet many patients neglect flossing, leading to plaque accumulation despite hydration efforts. In short, the guide scratches the surface but fails to address the multidisciplinary nature of dry‑mouth management.
Michael Coakley
December 2, 2025 AT 10:10Philosophically speaking, a dry mouth is just another reminder that the body is a mutable vessel, subject to the whims of medication and stress; the routine, while practical, merely patches the existential void.
ADETUNJI ADEPOJU
December 11, 2025 AT 16:24From a bioethical standpoint, prescribing a one‑size‑fits‑all regimen without acknowledging the pharmacodynamic interactions of antihistamines violates the principle of informed consent; moreover, the jargon‑laden recommendation to employ glycerin‑based moisturizers presumes a level of health‑literacy that is, frankly, unattainable for many patients.
Janae Johnson
December 20, 2025 AT 22:37While most agree that water intake is beneficial, I’d argue that the emphasis on “avoid caffeine” is a bit extreme; a moderate espresso in the morning can be part of a balanced regimen if followed by a rinse. Still, the core advice about soft brushing remains solid.
Kayla Charles
December 30, 2025 AT 04:50Honestly, when I first tried to follow a dry‑mouth routine, I felt like I was assembling a DIY spaceship; the steps seemed straightforward, but the reality quickly turned into a marathon of small adjustments. First, I learned that the amount of water you sip matters-a gulp of 150 ml is a great kickoff, but the real game changer is the consistency of that habit throughout the day. I started keeping a portable water bottle with me, setting reminders every hour, and soon the constant feeling of desert‑like tension in my cheeks faded. Then came the brush: switching to an ultra‑soft head felt like rubbing cotton on a pillow, and I stopped the inevitable bleeding that used to happen with regular bristles. The floss I used had a floss‑threader attached, which made reaching the back molars less of a chore. My toothpaste choice also evolved; I moved away from any that listed alcohol among the ingredients and gravitated toward a mild fluoride formula that didn’t sting. The mouthwash was a revelation-adding a xylitol‑rich, alcohol‑free rinse after brushing gave my mouth a subtle sweetness that lingered for hours. Chewing sugar‑free gum after meals turned into a mini workout for my salivary glands; I’d pick a mint flavor and chew for exactly fifteen minutes, watching the time on my phone. Water‑rich foods made their cameo in my snack drawer: cucumber slices, apple wedges, and watermelon cubes became my go‑to midday nibble. I also cut down on caffeine, not because I’m a zealot, but because I noticed that even a single latte could trigger a spike in dryness that lasted all afternoon. Over the weeks, the cumulative effect of these tiny tweaks was monumental: my speech became smoother, my taste buds revived, and I no longer felt the urgent need to lick my lips constantly. The plan, once a sterile list of bullet points, morphed into a personalized health strategy that respected my lifestyle while addressing the physiological challenges of xerostomia. In the end, the key takeaway is simple: consistency beats perfection, and a little creativity goes a long way in keeping your mouth comfortably moist.
Paul Hill II
January 8, 2026 AT 11:04Balancing hydration with practical daily habits is key; try setting a phone alarm for water breaks and keep a sugar‑free gum handy for those post‑meal moments.
Stephanie Colony
January 17, 2026 AT 17:17Only the truly discerning understand that a high‑quality saliva substitute is a privilege, not a mere convenience; if you’re not using the premium brand, you’re barely scratching the surface of oral care excellence.
Abigail Lynch
January 26, 2026 AT 23:30Everyone forgets that the government’s water fluoridation program is just a cover for nanoscale particles designed to control salivation; staying moisturized is a form of resistance.