
If you’ve had heartburn for years - even if it’s "mild" - you’re not just dealing with an annoying stomach issue. You might be at risk for something far more serious: esophageal cancer. The link between long-term acid reflux and this deadly cancer isn’t theoretical. It’s backed by hard data from large studies, and the timeline is clear: the longer you have GERD, the higher your risk becomes.
What GERD Does to Your Esophagus
Every time stomach acid backs up into your esophagus, it’s like a slow burn. Your esophagus isn’t designed to handle that kind of punishment. Over time, the body tries to protect itself by changing the lining of the esophagus. Instead of its normal squamous cells, it starts growing cells that look more like stomach lining. This is called Barrett’s esophagus, and it’s the only known precursor to esophageal adenocarcinoma, the most common type of esophageal cancer in the U.S.It sounds scary, but here’s the reality: most people with GERD never develop Barrett’s. Only about 5 to 15 out of every 100 people with chronic GERD will see this change. But if you’ve had acid reflux for five or more years - even if you’re on medication - your risk jumps. Studies show that people with long-term GERD are over three times more likely to develop esophageal cancer than those without it.
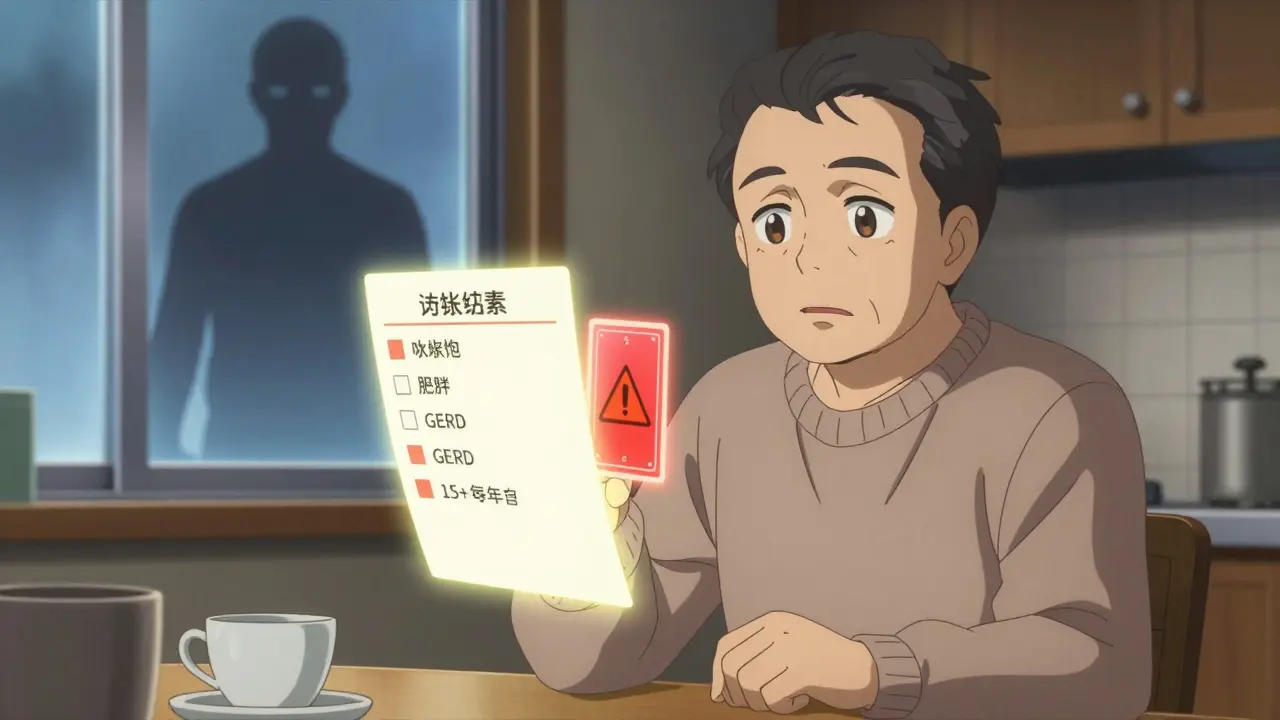
Who’s Really at Risk?
Not everyone with GERD is equally at risk. Certain factors stack up like dominoes. The biggest ones:- Male sex: Men are 3 to 4 times more likely than women to develop this cancer.
- Age 50+: Nine out of ten cases happen in people over 55.
- White, non-Hispanic ethnicity: White Americans have three times the rate of adenocarcinoma compared to Black Americans.
- Obesity: A BMI over 30 doubles or triples your risk. Fat around the abdomen pushes stomach contents upward.
- Smoking: Current or past smokers have 2 to 3 times higher risk.
- Family history: If a close relative had esophageal cancer, your risk goes up.
Combine even two or three of these, and your risk isn’t just higher - it’s sharply elevated. For example, a 60-year-old white man with obesity, a 15-year history of GERD, and a smoking history has a risk profile that doctors take very seriously.
Red Flags That Demand Immediate Attention
Most people with early-stage esophageal cancer feel fine. That’s why the warning signs are so critical. By the time symptoms appear, the cancer is often advanced. Don’t wait for pain. Watch for these six red flags:- Dysphagia: Feeling like food gets stuck in your chest or throat. It usually starts with solids - like bread or meat - then moves to liquids. This happens in 80% of diagnosed cases.
- Unexplained weight loss: Losing 10 pounds or more in six months without trying? That’s a major signal. It occurs in 60-70% of cases.
- Heartburn that won’t quit: If you’ve had heartburn more than twice a week for five or more years, you’re in the high-risk zone. Even if you think it’s "normal," it’s not.
- Food impaction: Food gets stuck so badly you need to drink water or even vomit to clear it. This happens in 30-40% of patients.
- Chronic hoarseness or cough: If your voice is raspy or you’ve had a persistent cough for over two weeks - especially if you’re not sick - get it checked. Acid can irritate your vocal cords.
- New reflux after age 50: If you never had heartburn before, but started having it after turning 50, especially with other risk factors, that’s a red flag.
These aren’t "maybe" signs. They’re urgent. The American Cancer Society says 75% of esophageal cancers are found at late stages because people ignore these symptoms. Don’t be one of them.
What Screening Can Do
The good news? If Barrett’s esophagus is caught early, you can stop cancer before it starts. The standard test is an upper endoscopy. A thin, flexible tube with a camera goes down your throat to check your esophagus. If Barrett’s is found, biopsies are taken to look for precancerous changes.Current guidelines from the American College of Gastroenterology recommend endoscopy for:
- White men over 50
- With chronic GERD (5+ years)
- Plus at least two other risk factors (obesity, smoking, family history)
Yet here’s the problem: only 13% of people who meet these criteria actually get screened. That’s a massive gap. If you fit this profile, don’t wait for symptoms. Talk to your doctor about screening.
How to Lower Your Risk
You’re not powerless. Even if you have GERD, you can cut your risk dramatically.- Quit smoking: Your risk drops by half within 10 years of quitting.
- Lose weight: Shedding 5-10% of your body weight cuts GERD symptoms by 40%. That’s not just about comfort - it’s cancer prevention.
- Limit alcohol: Stick to one drink a day for women, two for men. Heavy drinking increases a different type of esophageal cancer (squamous), but moderation helps overall.
- Take PPIs as prescribed: If you have Barrett’s esophagus, consistent use of proton pump inhibitors (like omeprazole or pantoprazole) for five or more years can reduce cancer risk by 70%.
- Don’t lie down after eating: Wait at least three hours after meals before going to bed. Elevate the head of your bed by 6-8 inches.
And here’s something surprising: treating GERD early doesn’t just help your stomach - it might prevent cancer. Studies show that early, consistent treatment can reduce the chance of developing Barrett’s esophagus by 40-60%.

The Bigger Picture
Esophageal adenocarcinoma is one of the fastest-rising cancers in the U.S. Since 1975, its incidence has jumped 850%. Why? Because obesity and GERD have exploded. In 1980, about 15% of Americans were obese. Today, it’s over 40%. More weight means more pressure on the stomach. More pressure means more acid reflux. More reflux means more Barrett’s. More Barrett’s means more cancer.But the survival rate tells a different story. If caught early - before it spreads - the 5-year survival rate is 50-60%. If it’s found late? It drops to under 20%. That’s why knowing your risk and acting early isn’t just smart - it’s life-saving.
New tools are coming. There’s a pill-sized sponge called the Cytosponge that you swallow. It collects cells from your esophagus and can detect Barrett’s with nearly 80% accuracy - no endoscopy needed. Researchers are also testing genetic markers that could predict who’s most likely to progress from GERD to cancer. But for now, the best tools are awareness and action.
Can GERD cause esophageal cancer even if I take medication?
Yes. Medications like PPIs reduce acid and help heal damage, but they don’t erase years of past exposure. If you’ve had GERD for five or more years - even while on medication - you still have an elevated risk of developing Barrett’s esophagus and, eventually, cancer. That’s why long-term GERD, not current symptoms, is the key factor.
I have GERD but no symptoms anymore. Am I still at risk?
Absolutely. Many people with Barrett’s esophagus have little to no heartburn. The damage has already been done. The cells have changed. That’s why silent GERD - reflux without obvious symptoms - is just as dangerous. Don’t assume symptom-free means risk-free.
Is esophageal cancer hereditary?
Family history matters. If a parent or sibling had esophageal cancer, your risk is higher. But it’s not like breast cancer genes. Most cases aren’t inherited. Instead, families often share lifestyle factors - diet, weight, smoking, or untreated GERD - that raise risk together. Still, if you have a family history, talk to your doctor about earlier screening.
How often should I get screened if I have Barrett’s esophagus?
It depends on the biopsy results. If no dysplasia (precancerous changes) is found, endoscopy is usually repeated every 3-5 years. If low-grade dysplasia is present, you’ll need endoscopy every 6-12 months. High-grade dysplasia often leads to treatment to remove the abnormal tissue. Your doctor will create a personalized plan based on your pathology.
Can I prevent Barrett’s esophagus if I’ve had GERD for years?
You can’t undo past damage, but you can stop it from getting worse. Quitting smoking, losing weight, taking PPIs as prescribed, and avoiding triggers like spicy foods or alcohol can significantly slow or halt progression. Studies show consistent PPI use reduces cancer risk by 70% in Barrett’s patients. Prevention isn’t about perfection - it’s about consistency.
What to Do Next
If you’re over 50, male, white, overweight, a smoker, and have had heartburn for five or more years - don’t wait. Make an appointment with a gastroenterologist. Ask about endoscopy. Bring your symptom history, medication list, and family health info.If you’re younger but have multiple risk factors and persistent symptoms - don’t brush it off. Keep a log: how often you have heartburn, what triggers it, whether swallowing is harder than before. That information helps your doctor decide if you need screening.
And if you’ve been told your reflux is "just stress" or "normal for your age" - get a second opinion. GERD isn’t normal. And it’s not harmless. The science is clear: chronic acid exposure changes your body. Early detection saves lives. Don’t ignore the warning signs - act on them.