Breathing Effort Calculator
Calculate Your Activity Effort
Use this tool to estimate breathlessness levels during daily activities based on occupational therapy principles. Input your current condition and activity to get personalized guidance.
Your Estimated Breathlessness Level
When it comes to breathing health, occupational therapy offers a hands‑on, everyday‑life approach that many people overlook. While doctors prescribe inhalers and physiotherapists focus on lung exercises, occupational therapists (OTs) dive into the routines that make up a person’s day-eating, dressing, commuting, and even sleeping-to keep the airway clear and the breath steady.
Key Takeaways
- Occupational therapy targets functional tasks, not just lung capacity.
- OTs use airway‑clearance techniques, adaptive equipment, and energy‑conservation strategies.
- A coordinated plan with pulmonologists, physical therapists, and speech‑language pathologists maximizes outcomes.
- Patients can start with a simple home‑based program after an OT assessment.
- Progress is tracked with tools like the Modified Borg Scale and pulmonary function tests.
Understanding Breathing Disorders
Breathing Disorders are medical conditions that impair the ability to move air in and out of the lungs efficiently. In the United States, chronic obstructive pulmonary disease (COPD) affects over 16 million adults, asthma touches roughly 25 million, and cystic fibrosis, though rarer, demands intensive daily airway management. These conditions share common challenges: reduced airflow, mucus buildup, and fatigue that spill over into everyday tasks like climbing stairs or cooking a meal.
Beyond the physiological impact, breathing disorders often trigger anxiety, limit social participation, and increase healthcare costs. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 report, effective multidisciplinary care can cut hospital readmissions by up to 30%.
What Occupational Therapy Brings
Occupational Therapy is a client‑focused health profession that helps individuals develop, recover, or maintain the skills needed for daily living and work. In the context of respiratory health, OTs assess how breathing difficulties affect functional performance and then design interventions that make everyday activities safer and less tiring.
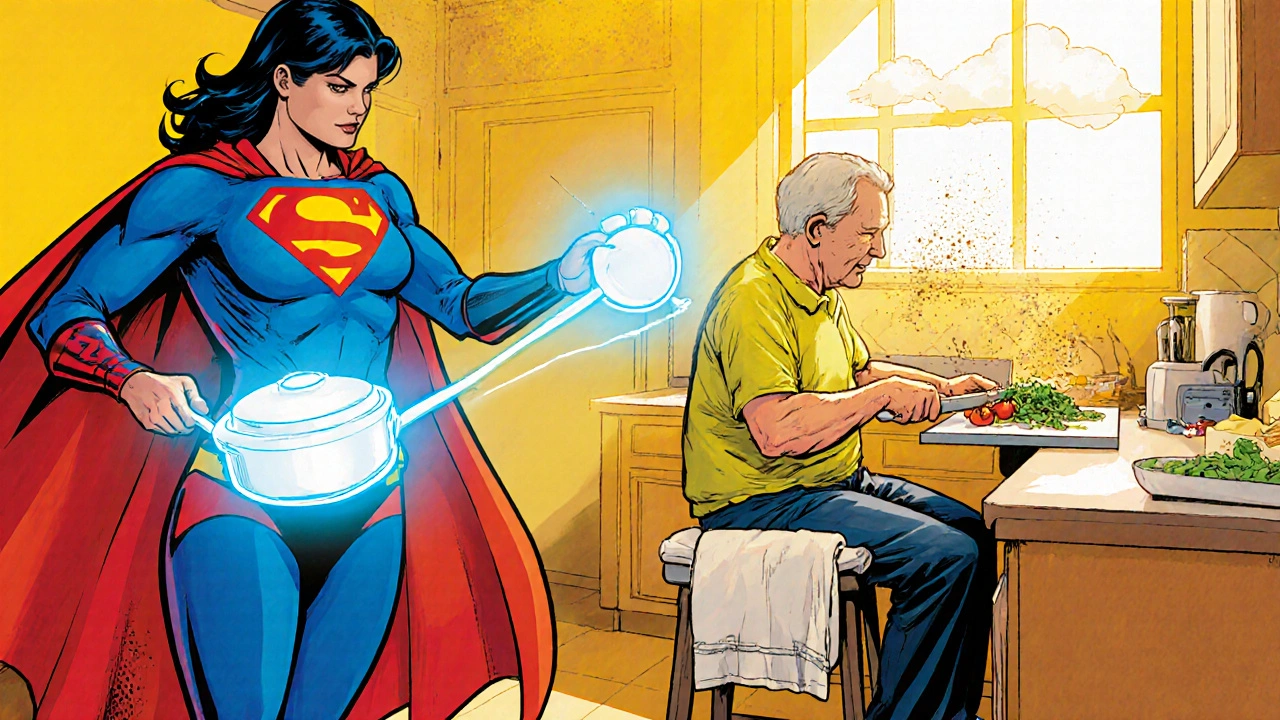
Rather than concentrating solely on lung mechanics, OTs look at the whole person: posture, environment, energy levels, and psychosocial factors. This holistic view allows them to address hidden barriers-like a poorly positioned home‑cooking setup that forces a person to lean forward, squeezing the diaphragm.
Core OT Interventions for Breathing Disorders
The toolbox includes several evidence‑based strategies, each tied to a specific functional goal.
- Airway Clearance Techniques (ACTs): Chest percussion, positive expiratory pressure (PEP) devices, and the “huff‑cough” method help move secretions out of the lungs. An OT will teach the patient to incorporate ACTs into toileting or bedtime routines.
- Energy Conservation Education: By re‑sequencing tasks, using timed‑breaks, and prioritizing essential activities, patients reduce breathlessness during daily chores.
- Adaptive Equipment Provision: Items such as long‑handled reachers, lightweight cooking utensils, and shower chairs minimize the need for excessive arm elevation, which can compromise breath control.
- Therapeutic Exercise: Tailored upper‑body conditioning (e.g., seated rowing) improves respiratory muscle endurance while staying within safe oxygen saturation limits.
- Positioning and Postural Training: Sitting upright or forward‑leaning positions open the thoracic cavity, making inhalation easier. OTs coach patients on optimal seating for reading, watching TV, or using a computer.
- Patient Education & Self‑Management: Instruction on inhaler technique, pacing, and recognizing early signs of exacerbation empower patients to act before a crisis.
How OT Works With Other Rehab Professionals
Collaboration is key. While pulmonologists manage medication and disease progression, physical therapists focus on aerobic conditioning, and speech‑language pathologists handle dysphagia and vocal cord function, OTs bridge the gap between medical treatment and daily life.
| Profession | Primary Focus | Typical Interventions | Key Outcome |
|---|---|---|---|
| Occupational Therapy | Functional performance | ACTs, adaptive equipment, energy conservation | Improved ADL independence |
| Physical Therapy | Mobility & endurance | Aerobic training, resistance exercises | Higher exercise tolerance |
| Speech‑Language Pathology | Airway protection & communication | Breathing coordination, voice therapy | Reduced aspiration risk |
| Pulmonology | Medical management | Medication, disease monitoring | Stabilized disease progression |
Getting Started: Referral, Assessment, and Goal‑Setting
The journey begins with a referral-often from a pulmonologist, primary‑care physician, or hospital discharge planner. Once the OT receives the referral, a comprehensive assessment follows:
- Medical Review: Diagnosis, medication list, recent exacerbations.
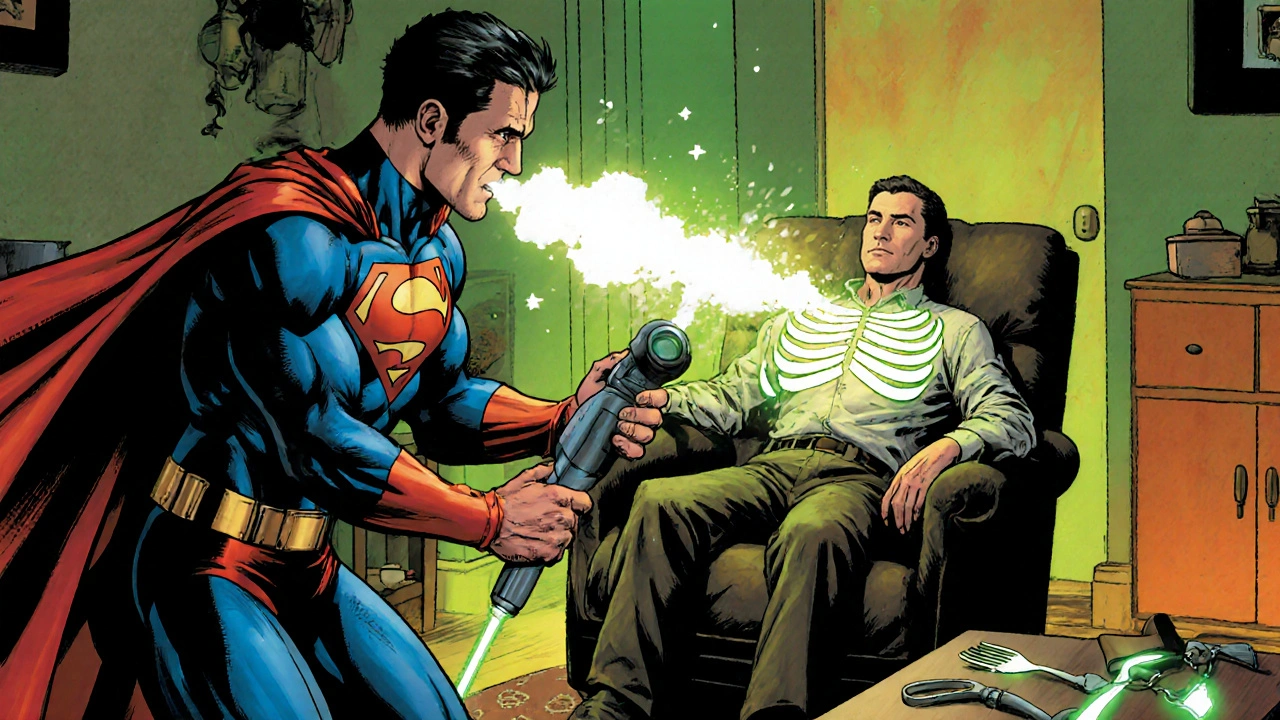
- Functional Screening: Observation of dressing, cooking, and mobility tasks while noting breath pattern and oxygen saturation.
- Environmental Scan: Home layout, bathroom safety, and workplace ergonomics.
- Patient Goals: Short‑term aims (e.g., “walk to the mailbox without stopping”) and long‑term aims (e.g., “return to part‑time gardening”).
Based on the findings, the OT crafts a personalized plan that blends ACTs, equipment, and habit restructuring. Sessions typically run 45‑60 minutes weekly for 6‑8 weeks, after which progress is re‑evaluated.

Practical Tips for Patients & Caregivers
- Integrate ACTs Into Routine: Perform chest percussion while watching a favorite TV show to make the practice stick.
- Use Timed‑Breaks: Follow the 1‑minute rest after every 5‑minute activity rule to keep oxygen levels stable.
- Choose the Right Tools: A lightweight, ergonomically‑designed kitchen set reduces arm elevation, lessening breathlessness.
- Maintain Good Posture: Place a rolled towel behind the lower back while seated to open the chest cavity.
- Track Symptoms: A simple diary noting Borg Scale scores, sputum volume, and activity tolerance helps the OT adjust the program.
Measuring Success: Outcomes & Evaluation Tools
OTs rely on both subjective and objective metrics.
- Modified Borg Dyspnea Scale: Rates breathlessness from 0 (no breathlessness) to 10 (max breathlessness) during activities.
- Six‑Minute Walk Test (6MWT): Tracks distance covered in six minutes, reflecting functional endurance.
- Canadian Occupational Performance Measure (COPM): Captures patient‑reported performance and satisfaction scores for selected daily tasks.
- Pulmonary Function Tests (PFTs): FEV1 and FVC values, recorded by the medical team, help correlate functional gains with lung capacity.
When these indicators improve-say, a drop of two points on the Borg Scale while cooking or an extra 30meters on the 6MWT-the OT knows the plan is working and can set new challenges.
Frequently Asked Questions
Can occupational therapy replace medication for breathing disorders?
No. OT complements medication and medical management. It helps you do everyday tasks more comfortably while drugs target the underlying disease.
How often will I see an OT?
Most programs start with weekly 45‑minute sessions for six to eight weeks, then shift to monthly check‑ins or a home‑exercise schedule.
Do I need special equipment?
Your OT will recommend only what you truly need-often simple items like a reacher, a lightweight utensil, or a PEP device. Many tools are covered by insurance when prescribed.
Is OT covered by Medicare or private insurers?
Yes, most plans cover OT when it’s ordered by a physician for a documented breathing disorder. Check your policy for any referral requirements.
What should I bring to my first OT appointment?
Bring your medication list, recent lung function test results, a diary of daily symptoms, and any devices you already use (inhalers, oxygen equipment). Wear comfortable clothing you can move in.
Lindsey Bollig
August 1, 2025 AT 00:13Occupational therapy can totally make daily chores feel less breath‑heavy.
Daniel Buchanan
August 5, 2025 AT 15:20Hey everyone, just wanted to add that OT isn’t just about exercises – it’s about tweaking everyday habits so you waste less energy and breathe easier. Think of it like a personal coach for your daily routine.
Lena Williams
August 10, 2025 AT 06:26Okay so I was reading the article and I gotta say it really opened my eyes to how many tiny things we do that actually make breathing harder, especially when you have COPD or asthma, and that’s kinda wild because most of us just think about meds and inhalers, not about how we reach for a pot on the top shelf or how we bend over to tie our shoes, which can totally cramp the diaphragm.
Like, you can actually set up your kitchen so everything you need is within arm’s reach, that means less leaning forward and less pressure on your lungs, and that’s a game‑changer for people who get winded just opening a fridge.
Also, the whole idea of timed‑breaks, like a minute rest after five minutes of activity, is something you can actually practise while watching a TV show – you just stand up, stretch, take a few deep breaths, and then sit back down.
And don’t forget about the ACTs, those chest percussion things – you can do them while you’re watching Netflix, just a little tap‑tap on your back, and it helps clear mucus without a big fuss.
It’s also cool that OTs look at posture – sitting up straight while you read or use a laptop opens up your chest cavity, which lets more air into your lungs, which is something we never think about because we just sit slouched.
Honestly, I think the biggest takeaway is that OT is all about making the little tweaks in your environment – like swapping heavy pots for lighter ones, using a reacher for shelves, or putting a stool in the shower – that can save you a ton of breath they’re talking about.
Also, the article mentions using a PEP device, and while it sounds fancy, it’s just a simple tool that helps you exhale against resistance, which can keep your airways clear and improve oxygen exchange.
Overall, the holistic approach of OT that blends equipment, positioning, and pacing is a real lifesaver for folks dealing with chronic breathing issues, and it’s way more accessible than you’d think.
Sierra Bagstad
August 14, 2025 AT 21:33The article correctly emphasizes that occupational therapy addresses functional performance, not merely pulmonary metrics. By integrating airway clearance techniques, adaptive equipment, and energy‑conservation strategies, OTs facilitate measurable improvements in ADL independence, as evidenced by reductions in Borg Scale scores and increased 6MWT distances.
Alan Kogosowski
August 19, 2025 AT 12:40From a clinical perspective, the multi‑disciplinary synergy described showcases the nuanced role of occupational therapy within respiratory care. While physiotherapists target aerobic capacity, the OT’s focus on task‑specific adaptations-such as long‑handled reachers and optimized seating postures-directly mitigates dyspnea during daily activities. Moreover, the emphasis on patient‑centered goal setting aligns with contemporary rehabilitation models, ensuring that interventions are both relevant and sustainable. It is also worth noting that the incorporation of the Modified Borg Scale provides a reliable subjective measure that can be tracked longitudinally, offering clinicians actionable data to fine‑tune therapy plans. In practice, this translates to a reduction in hospital readmissions, a metric that healthcare systems worldwide are striving to improve.
David Brice
August 24, 2025 AT 03:46Look, I get that OT is “nice” and all, but if you’re not actually putting in the work you’ll see no change – you gotta push yourself, use the equipment, and follow the schedule. Don’t just sit there and expect miracles.
Zachary Schroer
August 28, 2025 AT 18:53Honestly this whole OT hype is just a trendy buzzword for basic ergonomics 🙄🧐. Sure, posture matters, but calling it a breakthrough is a bit pretentious. People could benefit from a simple chair adjustment without needing a whole therapy plan.
Adrian Hernandez
September 2, 2025 AT 10:00While everyone is raving about “simple chair adjustments,” what they don’t tell you is how these recommendations come from the same health‑industry elite pushing invisible agendas. The real motive is to keep us reliant on proprietary equipment sold by big corporations.
duncan hines
September 7, 2025 AT 01:06Oh great, now we’re blaming the whole system because a therapist suggested a stool. Drama much? Let’s not forget the actual science behind OT – it’s not a conspiracy, it’s proven to help folks breathe easier.
Geneva Lyra
September 11, 2025 AT 16:13I totally agree that this article shows how OT can bridge cultures – different households have different routines, and a therapist can respect those while suggesting small changes. It’s all about collaboration and respecting each person’s background.
Tim Ferguson
September 16, 2025 AT 07:20People keep saying OT is just “nice,” but think about it: it’s about making life possible when you can’t breathe easy. Simple changes, big impact.
Noah Cokelaere
September 20, 2025 AT 22:26Sure, “big impact,” but only if you actually follow the plan. Otherwise it’s just a fancy way of saying “stand up and breathe.”
Brian Jones
September 25, 2025 AT 13:33All right, let’s break this down:; OT provides concrete tools; it empowers patients; it complements medical treatment; and, most importantly, it respects individual pacing-yes, even if that pacing feels a bit slow at first!.