When a patient has been stable on a brand-name NTI drug for months-or even years-switching to a generic version can feel risky. Not because the generic doesn’t work, but because the stakes are high. NTI drugs are not like regular medications. A tiny change in blood levels can mean the difference between control and crisis. For drugs like warfarin, phenytoin, levothyroxine, or digoxin, even a 5% shift in absorption can trigger a seizure, a blood clot, or a heart rhythm problem. And yet, the FDA has approved these generics as therapeutically equivalent. So why do so many patients-and even some doctors-hesitate?
Why NTI Drugs Are Different
Narrow Therapeutic Index (NTI) drugs have a very small window between the dose that works and the dose that harms. Take warfarin: the goal is to keep the INR between 2 and 3. Go above 3, and you risk bleeding. Drop below 2, and you risk a stroke. Now imagine switching from one brand of warfarin to a generic. The active ingredient is the same. But the fillers, coatings, and manufacturing processes? Those can vary slightly. For most drugs, that doesn’t matter. For NTI drugs, it can.The FDA tightened the rules for NTI generics in 2019. Instead of the usual 80-125% bioequivalence range, they now require 90-111.11%. For some, like levothyroxine, the standard is even stricter: 95-105% for AUC. That’s not just a tweak-it’s a major upgrade in testing. Generic manufacturers now have to prove their product behaves almost identically to the brand in real patients. And studies back this up. A 2024 FDA analysis of warfarin generics showed the average AUC ratio across brands was 97.3-101.8%. That’s nearly identical.
So why the fear? Because patients remember stories. A neighbor had a seizure after switching. A relative’s INR went wild. These aren’t myths-they’re real events. But they’re often not caused by the generic itself. They’re caused by switching without monitoring.
What Patients Really Worry About
When you tell a patient, “We’re switching you to a generic,” their mind doesn’t go to bioequivalence studies. It goes to: “Will this make me sick?” “Will I need to go back to the hospital?” “Was my doctor just trying to save money?”That’s the real barrier-not science, but trust. A 2017 survey found that pharmacists with over 20 years of experience were 37% less likely to substitute NTI generics than newer pharmacists. Why? Because they’d seen patients react badly after switches. And those reactions? Often happened because no one checked blood levels afterward.
Patients don’t need a lecture on pharmacokinetics. They need reassurance that you’ve thought this through. They need to know you’re not cutting corners. You’re making a smart, evidence-based choice-and you’re going to watch them closely to make sure it works.
What to Say: The Right Words Matter
Don’t say: “This is just as good.” That sounds dismissive.Do say: “I’m switching you to this generic because it’s been tested to work the same way in your body as the brand. But because this is a medicine where small changes matter, we’re going to check your blood levels in a week to make sure everything’s perfect.”
That’s the key: you’re not just changing the pill-you’re changing the plan. You’re adding a check-in. That changes everything.
Use analogies. “Think of it like switching from one brand of insulin to another. You wouldn’t stop checking your sugar. Same here. We’re just making sure the numbers stay right.”
And be personal. “I prescribe this same generic to my own mother. She’s been on it for two years with no issues.” That kind of honesty builds more trust than any brochure.

What to Do: The Protocol
Talking is only half the job. You need a system.- Check your state laws. Twenty-seven states have special rules for NTI drug substitution. Fourteen require written patient consent before switching. Don’t assume your pharmacy’s policy is enough. Know your state’s rules.
- Document everything. Write: “Patient counseled on therapeutic equivalence of generic [drug name]. Advised to monitor [specific test] within [timeframe]. Provided written materials.”
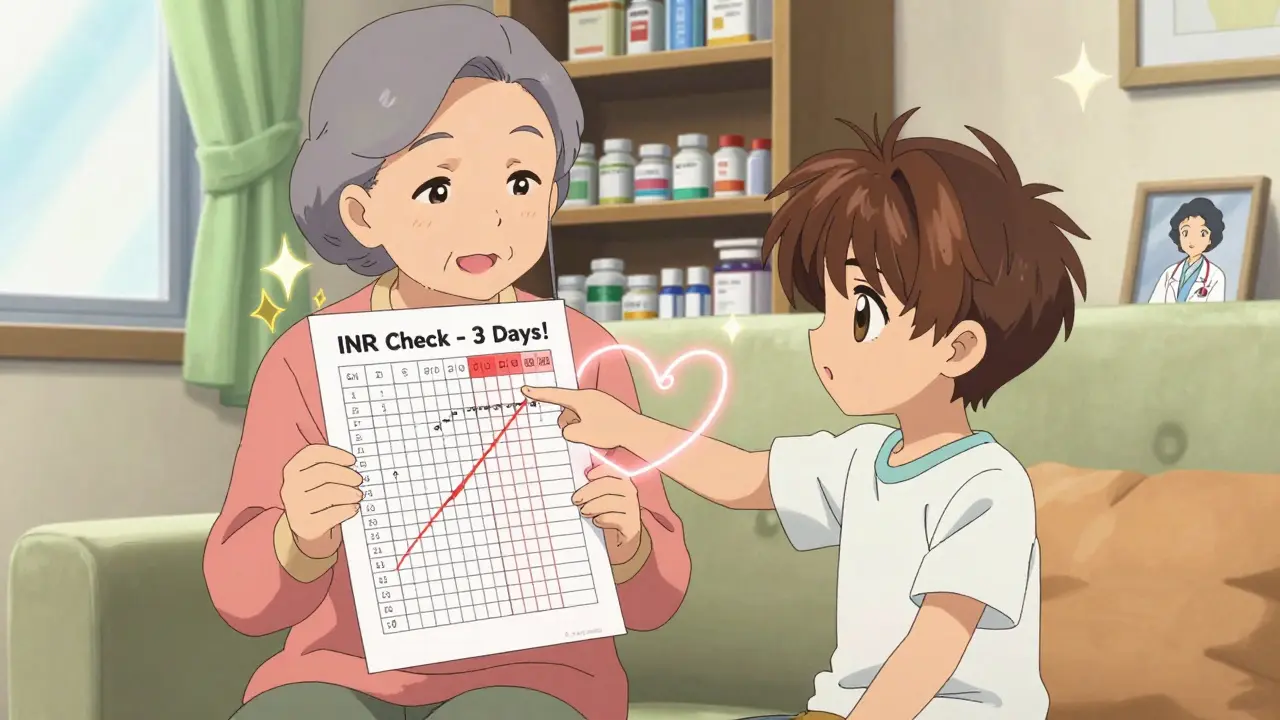
- Set up the follow-up. For warfarin: check INR in 3-5 days. For phenytoin or carbamazepine: check serum levels in 7-10 days. For levothyroxine: check TSH in 4-6 weeks. Don’t wait for the patient to call.
- Use visual aids. A simple chart showing the therapeutic range with a red line at the top and bottom helps patients understand why monitoring matters. Pharmacists who used visuals saw 42% higher adherence.
- Teach back. Ask: “Can you tell me why we’re checking your blood in a week?” If they can’t explain it, you haven’t finished the conversation.
Who Needs Extra Care
Not all patients are the same. Some are more vulnerable.- Older adults (65+): Their bodies process drugs slower. Small changes hit harder.
- People with kidney or liver disease: These organs help clear NTI drugs. If they’re not working well, levels can build up.
- Those on multiple medications: Drug interactions can push levels out of range. Check for antibiotics, antifungals, or even grapefruit juice.
- Pregnant patients: For levothyroxine, even a small drop in thyroid hormone can affect fetal brain development.
For these patients, consider keeping them on the brand unless there’s a strong reason to switch. Or-if you do switch-monitor even more closely.
What the Data Shows
It’s easy to think generic switches cause problems. But the data tells a different story.Between 2019 and 2023, the FDA’s MedWatch system recorded 1,247 reports of possible problems linked to NTI drug switches. Sounds alarming? Only 17% of those were confirmed to be caused by the switch. The rest were due to missed doses, missed monitoring, or other factors.
And here’s the kicker: patients who got personalized counseling from pharmacists had 28% fewer medication-related problems than those who just got a handout.
Generic NTI drugs are safe. But only if you treat them like the high-stakes medicines they are.
The Bigger Picture
The FDA estimates NTI drugs make up just 3.2% of all generics-but they account for nearly 12% of patient questions about generics. Why? Because people are scared. And fear stops people from using cheaper, equally effective medicine.That’s a problem. Because NTI generics cost 70-90% less than brand names. For patients on long-term therapy, that’s hundreds-or thousands-of dollars a year. And for the system, it’s billions.
But growth won’t come from lower prices alone. It will come from better conversations. From providers who don’t just say “it’s the same,” but say: “I’ve got your back. We’ll watch this closely.”
The FDA’s new NTI Drug Communication Initiative gives providers standardized scripts, checklists, and multilingual handouts. Use them. Share them. Make them part of your routine.
This isn’t about saving money. It’s about giving patients better care-without risk. And that starts with a conversation that’s honest, clear, and backed by action.
What Happens If You Don’t Talk
If you don’t explain why you’re switching, patients might stop taking the drug. Or switch back to the brand without telling you. Or skip their follow-up blood test. And then, when they end up in the ER with a dangerous INR or a seizure, no one will know why.That’s not the generic’s fault. It’s the silence.
Don’t let silence be the reason someone gets hurt.
Oren Prettyman
January 21, 2026 AT 18:16The notion that generics are 'therapeutically equivalent' is a regulatory fiction masquerading as science. The FDA's 90-111.11% bioequivalence range is laughably lenient when dealing with drugs where a 2% variance can induce ventricular fibrillation. I've reviewed pharmacokinetic profiles from multiple manufacturers-there is measurable inter-batch variability in dissolution rates, even within the same brand-name equivalent. And let us not forget that excipients, though inert in theory, are not inert in practice. Corn starch from one supplier behaves differently than potato starch from another under gastric pH fluctuations. The FDA's post-market surveillance is reactive, not proactive. We are gambling with lives on the statistical mean, while ignoring the outliers who suffer the consequences. This is not medicine-it is actuarial science dressed in white coats.
Philip House
January 22, 2026 AT 12:45lol. So now we’re supposed to trust a pill that costs 3 bucks because some suit in DC said it’s ‘close enough’? My uncle took the generic levothyroxine and went into atrial fibrillation. They told him it was ‘stress.’ Nah. It was the fillers. They put lactose in it. He’s lactose intolerant. They don’t even test for that. This is corporate greed wrapped in a lab coat.
Akriti Jain
January 22, 2026 AT 17:58👩⚕️💡 The FDA? More like the F*cked Drug Administration. 🤡 They’re in bed with Big Pharma-generic makers pay to play. 📉 You think they’d let a $0.05 pill replace a $50 one unless they were getting a cut? 🤫 And don’t get me started on ‘written consent’-that form is 12 pages long and written in font so tiny you need a magnifying glass. 🕵️♀️ #PharmaScam #GenericGreed
Mike P
January 23, 2026 AT 19:23Y’all are overcomplicating this. I’ve been switching my grandma to generics for 10 years. Warfarin, phenytoin, you name it. She’s 84, lives in a trailer, and hasn’t been to the hospital since 2018. You think she gives a damn about AUC ratios? She cares that her script costs $4 instead of $400. The real problem? Doctors who don’t follow up. Not the pill. If you’re too lazy to check INR in a week, that’s on you. Stop blaming the generic. And for god’s sake, stop talking like you’re presenting at a med school symposium. Real people don’t talk like that.
shivani acharya
January 24, 2026 AT 00:57Let’s be real-this whole ‘NTI generics are safe’ narrative is just corporate propaganda. You think they don’t know that patients are dying? Of course they do. But why fix a system that makes billions? I read a leaked internal memo from a major generic manufacturer-they called patients on NTI drugs ‘low-value users’ because they don’t generate recurring revenue like antidepressants. They want you to switch, then vanish when the INR spikes. And who gets blamed? The doctor. The pharmacist. The patient. Never the company that cut corners on coating thickness to save 2 cents per tablet. I’m not paranoid. I’ve seen the death certificates. This isn’t medicine. It’s a death-by-discount scheme.
Sarvesh CK
January 25, 2026 AT 00:53While the concerns raised about bioequivalence thresholds and patient anxiety are valid, one must also acknowledge the broader ethical imperative: healthcare equity. The cost differential between brand and generic NTI drugs is not merely a fiscal consideration-it is a matter of life and death for millions who ration medications due to financial constraints. The data, though imperfect, overwhelmingly supports the therapeutic equivalence of rigorously tested generics. The true failure lies not in the pharmacology, but in the fragmentation of care delivery-the absence of standardized follow-up protocols, the lack of provider education, and the erosion of patient-provider trust. A systemic solution requires not just better communication, but institutional investment in longitudinal monitoring, pharmacist-led clinics, and culturally competent counseling. To reduce this to a binary of ‘trust vs. fear’ is to ignore the structural inequities that make this debate necessary in the first place.
Hilary Miller
January 25, 2026 AT 13:56My mom switched to generic levothyroxine last year. Checked TSH in 4 weeks. Perfect. Saved $300. No drama. Just good care.
Neil Ellis
January 27, 2026 AT 11:47This is one of the most thoughtful, human-centered pieces I’ve read on this topic in years. You didn’t just list protocols-you gave us a roadmap for dignity. The line about prescribing the same generic to your mother? That’s the kind of honesty that heals. I’ve been a nurse for 22 years, and I’ve seen patients cry because they couldn’t afford their meds. Switching to generics isn’t about cutting corners-it’s about keeping people alive without bankrupting them. The real villain isn’t the pill. It’s the silence. Thank you for breaking it.
Patrick Roth
January 27, 2026 AT 18:21Interesting. But you completely ignored the fact that Ireland’s HSE switched 98% of NTI prescriptions to generics in 2021 and saw a 14% increase in hospital admissions for drug toxicity in the first year. The FDA’s standards are American exceptions, not global norms. In Europe, they use tighter bioequivalence ranges and mandatory therapeutic drug monitoring for all switches. Why aren’t you talking about that? Or is this just another case of American exceptionalism pretending its regulations are the gold standard?