
Vitamin Deficiency Risk Assessment Tool
Answer these questions to see which vitamin deficiencies might be contributing to your headaches.
Your Vitamin Deficiency Risk Assessment
Recommended Next Steps:
Important Note:
This tool provides general information only. Always consult with a healthcare professional for proper diagnosis and treatment.
If you suffer from headaches, checking your vitamin levels could be the missing piece of the puzzle. While stress, dehydration, and lack of sleep are well‑known culprits, hidden nutritional gaps often slip under the radar. This guide breaks down the science behind the link, shows which vitamins matter most, and gives you clear steps to protect your brain from avoidable pain.
What are Headaches is a symptom characterized by pain in any region of the head, ranging from occasional tension to severe migraine attacks?
Headaches are far more than a nuisance; they can signal underlying health issues. Primary types include tension‑type headaches, cluster headaches, and migraines. Tension‑type headaches usually cause a dull, band‑like pressure, while migraines bring throbbing pain often accompanied by nausea, light sensitivity, and visual disturbances. Understanding the type you experience helps pinpoint triggers, including nutritional deficits.
What is a Vitamin Deficiency is a condition where the body lacks sufficient amounts of essential vitamins needed for normal physiological functions?
Vitamins are organic compounds the body cannot produce in adequate quantities, so we must obtain them from food or supplements. A deficiency can disrupt enzyme activity, neurotransmitter balance, and blood flow-all critical for brain health. When a vitamin shortfall affects nerve signaling or vascular tone, headaches can emerge as an early warning sign.
Which vitamins are most commonly tied to headache symptoms?
- Magnesium is an essential mineral that regulates nerve function, muscle relaxation, and blood vessel tone. Low magnesium levels are linked to migraine frequency and severity.
- Vitamin D is a fat‑soluble vitamin that supports calcium metabolism and modulates immune responses. Deficiency may increase inflammation, a known migraine trigger.
- Vitamin B12 is a water‑soluble vitamin crucial for red blood cell formation and nervous system maintenance. Insufficient B12 can cause neuropathic pain that mimics headache patterns.
- Iron is a mineral required for oxygen transport in the blood. Iron‑deficiency anemia reduces oxygen delivery to the brain, leading to pressure‑type headaches.
- Riboflavin (Vitamin B2) is a B‑vitamin involved in mitochondrial energy production. Studies show riboflavin supplementation can reduce migraine days.
- Folate is a B‑vitamin (B9) that aids DNA synthesis and neurotransmitter balance. Low folate levels have been observed in chronic migraine sufferers.
- Omega‑3 fatty acids is essential polyunsaturated fats that reduce inflammation and support neuronal health. A diet low in omega‑3s may exacerbate headache intensity.
How do these deficiencies actually cause a headache?
Each vitamin influences the nervous system in a slightly different way. Magnesium, for example, blocks the release of certain neurotransmitters that can trigger migraine cascades. Without enough magnesium, blood vessels may spasm, leading to the classic pulsating migraine pain. Vitamin D deficiency heightens inflammatory cytokines, which can sensitize trigeminal nerves-a key pathway for migraine.
Vitamin B12 and iron are tied to oxygen and blood health. A shortage reduces hemoglobin production, limiting oxygen to brain tissue and causing a dull, pressure‑filled headache. Riboflavin and folate support mitochondrial energy; when mitochondria run low on fuel, neurons become hyper‑excitable and more prone to firing pain signals.

Red flags: Signs your headaches might be nutrition‑related
Not every ache points to a vitamin problem, but look for patterns that suggest a deficiency:
- Headaches that improve after a balanced meal or a nutrient‑rich snack.
- Co‑occurring symptoms such as fatigue, muscle twitches (magnesium), pale skin (iron), or tingling in the hands and feet (B12).
- Seasonal spikes-vitamin D deficiency often worsens in winter months when sunlight exposure drops.
- Family history of migraine combined with poor dietary habits.
Testing: How to confirm a vitamin deficiency
Blood tests are the gold standard. Ask your doctor for a comprehensive panel that includes serum magnesium, 25‑OH vitamin D, ferritin (iron storage), vitamin B12, and RBC folate. For riboflavin, a urine test measuring its metabolite (EGR) can be used, though it’s less common. Results typically show whether you’re below the recommended range, guiding targeted supplementation.
Dietary strategies: Boosting your vitamin intake naturally
Before reaching for pills, consider food‑first approaches. Here’s a quick reference:
- Magnesium: leafy greens (spinach, Swiss chard), nuts (almonds, cashews), seeds (pumpkin), whole grains, and dark chocolate.
- Vitamin D: fatty fish (salmon, mackerel), fortified dairy or plant milks, egg yolks, and regular safe sunlight exposure (10‑15 minutes a few times a week).
- Vitamin B12: animal products (beef liver, clams, poultry), fortified cereals for vegans.
- Iron: red meat, lentils, chickpeas, tofu, quinoa, and vitamin C‑rich foods (citrus, bell peppers) to enhance absorption.
- Riboflavin: dairy, eggs, almonds, and enriched breads.
- Folate: dark leafy greens, avocado, beans, and fortified grains.
- Omega‑3: salmon, sardines, chia seeds, flaxseeds, and walnuts.
Pair iron‑rich foods with vitamin C sources to improve uptake, and avoid excessive coffee or tea around magnesium‑rich meals, as these drinks can hinder absorption.
Supplementation: When food isn’t enough
If blood work confirms a deficit, targeted supplements are a practical next step. Choose high‑quality, third‑party‑tested products. Typical dosages based on recent clinical guidelines are:
- Magnesium citrate or glycinate: 300‑400 mg daily (split into two doses to improve tolerance).
- Vitamin D3: 1,000‑2,000 IU daily, or higher under physician supervision for severe deficiency.
- Vitamin B12 (cyanocobalamin or methylcobalamin): 1,000 µg sublingual weekly or 500 µg daily.
- Iron (ferrous sulfate): 65 mg elemental iron once daily, taken with food to reduce stomach upset.
- Riboflavin: 400 mg daily, a dose shown to cut migraine frequency in several trials.
- Folate: 400‑800 µg daily.
- Omega‑3 (EPA/DHA): 1,000 mg combined daily.
Always discuss supplementation with a healthcare provider, especially if you take other medications, as interactions (e.g., between iron and certain antibiotics) can occur.
When to seek professional help
Even with optimal nutrition, some headaches demand medical evaluation. See a doctor if you experience any of the following:
- Sudden, severe “thunderclap” pain.
- New onset after age 50.
- Neurological signs such as weakness, vision loss, or speech difficulties.
- Headaches that progressively worsen despite lifestyle changes.
- Persistent nausea, vomiting, or fever accompanying the pain.
These symptoms could signal conditions unrelated to nutrition, like aneurysms, infections, or medication overuse.
Quick reference: Common Vitamin Deficiencies Linked to Headaches
| Vitamin/Mineral | Typical Deficiency Symptoms | Headache Type Most Linked | Recommended Daily Intake (Adults) |
|---|---|---|---|
| Magnesium | Muscle cramps, fatigue, anxiety | Migraine | 310‑420 mg |
| Vitamin D | Bone pain, fatigue, mood swings | Migraine, tension‑type | 600‑800 IU |
| Vitamin B12 | Tingling, memory issues, anemia | Neuropathic‑type headache | 2.4 µg |
| Iron | Pale skin, shortness of breath, restless legs | Pressure‑type headache | 8‑18 mg |
| Riboflavin (B2) | Cracked lips, sore throat, dermatitis | Migraine | 1.1‑1.3 mg |
| Folate | Fatigue, irritability, macrocytic anemia | Migraine | 400 µg |
| Omega‑3 | Dry skin, joint stiffness, mood swings | Inflammatory migraine | 250‑500 mg EPA+DHA |
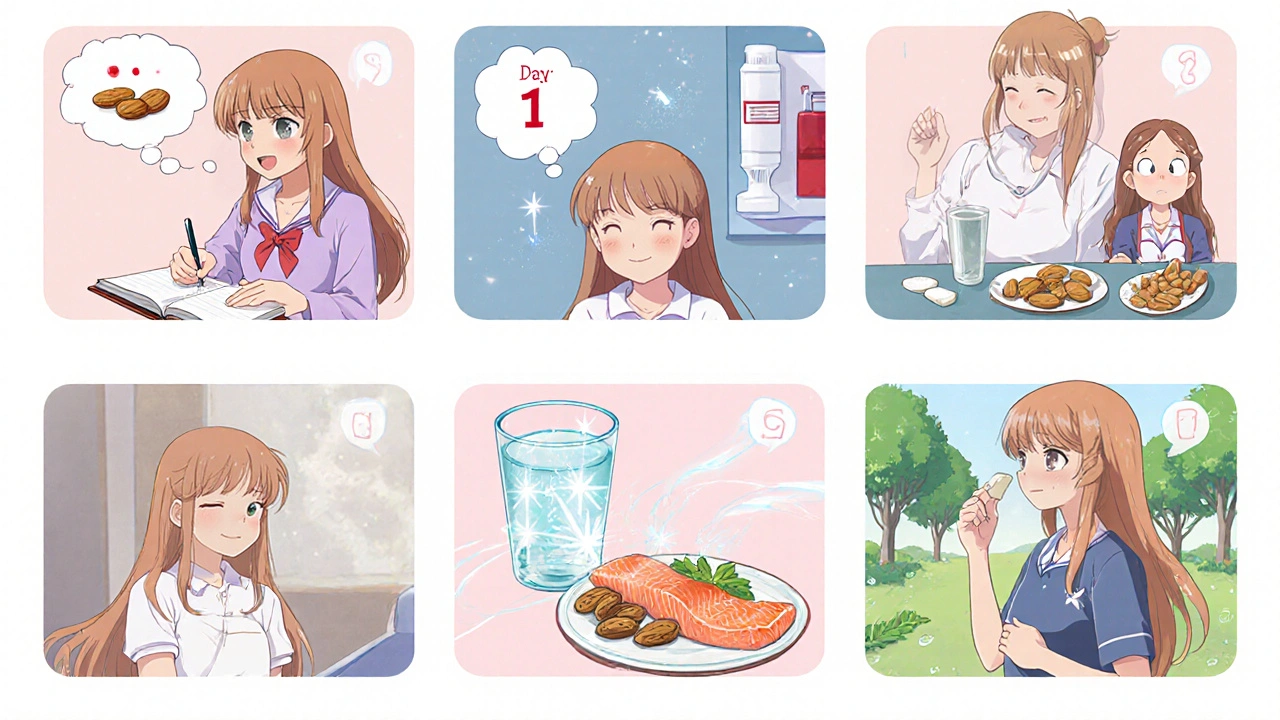
Putting it all together: Your 7‑Day Headache‑Proof Plan
- Day 1 - Assess: Keep a simple diary noting headache timing, food intake, sleep, and stress.
- Day 2 - Test: Schedule a blood panel for magnesium, vitamin D, B12, iron, and folate.
- Day 3 - Eat: Add a magnesium‑rich snack (a handful of almonds) and a vitamin D source (grilled salmon).
- Day 4 - Supplement: If labs show low magnesium, start a 300 mg magnesium glycinate supplement.
- Day 5 - Hydrate: Aim for 2‑2.5 L of water; dehydration can mask deficiency symptoms.
- Day 6 - Move: Light aerobic exercise improves circulation and helps the body utilize nutrients.
- Day 7 - Review: Re‑check your diary. If headaches persist, consult a healthcare professional for further evaluation.
This short cycle isn’t a cure‑all, but it gives you a structured way to address nutritional gaps that often hide behind everyday headaches.
Can a single vitamin deficiency cause chronic migraines?
Yes. Research shows that low magnesium or vitamin D levels can increase migraine frequency. Correcting the deficiency often reduces attack days, though results vary per individual.
How long does it take to see improvement after starting supplements?
Most people notice a change within 4‑6 weeks for magnesium and riboflavin, while vitamin D may require 8‑12 weeks to reach optimal blood levels.
Should I test for all vitamins at once?
A targeted panel based on symptoms is more cost‑effective. Commonly tested are magnesium, vitamin D, B12, iron, and folate. Your doctor can add others if needed.
Are there risks to taking too much magnesium?
High doses (over 350 mg from supplements) can cause diarrhea or stomach upset. Very large amounts may lead to low blood pressure, so stick to recommended doses and talk to a clinician.
Can diet alone fix a vitamin D deficiency?
Often not. Food sources provide limited vitamin D; sensible sunlight exposure plus a modest supplement is usually required to reach optimal blood levels.
Harini Prakash
October 22, 2025 AT 16:52Thanks for sharing this detailed guide :) It’s amazing how something as simple as a magnesium‑rich snack can make a real difference in migraine frequency. I’ve started adding a handful of almonds and a bit of dark chocolate after lunch and noticed my tension‑type headaches are less intense. Keeping a food‑and‑pain diary, as you suggested, really helps pinpoint which nutrients are missing. Hope everyone gives these tips a try and feels the relief soon.
Rachael Turner
October 24, 2025 AT 04:59Interesting perspective on magnesium and diet it feels like a small tweak can ripple into big changes For me the link between vitamin D and seasonal mood swings also ties into headache patterns I’ve been trying to catch more sunlight in winter and notice less throbbing after a few weeks It’s cool how the body balances these nutrients without us always realizing It reminds us to look beyond caffeine and stress when the pain strikes
Tiffany Davis
October 25, 2025 AT 17:05I’ve found iron deficiency can really worsen pressure headaches, especially if you’re not getting enough vitamin C with meals.
Bret Toadabush
October 27, 2025 AT 04:12Yo the pharma lords don’t want u knowin’ that iron pills are just placebos they push synthetic supplements that make ya dependent. Real food like liver and beans are the truth they hide. Wake up!
Diane Thurman
October 28, 2025 AT 16:19Honestly this whole “just eat more greens” thing is overrated. Most people cant even stick to a diet, let alone track vitami levels. If you’re still having headaches after these tricks you probably have something else going on. Maybe see a specialist instead of scrolling forums.
Iris Joy
October 30, 2025 AT 04:25First, get a baseline laboratory panel that includes serum magnesium, 25‑hydroxy vitamin D, ferritin, vitamin B12, and red‑blood‑cell folate – these are the most common culprits in nutrient‑related headaches. Once you have the results, compare each value to the reference range and note any deficiencies; even a borderline low level can be clinically significant when it comes to neuronal function. If magnesium is below 1.8 mg/dL, consider a split dose of 200 mg magnesium glycinate twice daily, as this form has better absorption and less gastrointestinal upset. For vitamin D insufficiency (25‑OH level under 30 ng/mL), a loading phase of 5,000 IU daily for six weeks often brings levels into the optimal range, followed by a maintenance dose of 1,000‑2,000 IU. Should B12 be low, a weekly 1,000 µg sublingual dose or a daily 500 µg oral supplement can quickly replenish stores and improve neuropathic symptoms. Iron deficiency anemia requires an elemental iron dose of about 65 mg daily, taken with a vitamin C source such as orange juice to enhance absorption, and it’s wise to monitor ferritin after eight weeks. Folate supplementation of 400‑800 µg daily supports methylation pathways and may reduce migraine frequency, especially when combined with B12. Riboflavin at 400 mg per day has solid evidence for decreasing migraine days, so add a high‑quality B2 supplement if your diet lacks dairy and eggs. Omega‑3 fatty acids, preferably as a combined EPA/DHA supplement of 1,000 mg daily, help dampen inflammatory processes that can sensitize the trigeminal nerve. Alongside supplements, adjust your diet to include magnesium‑rich foods like spinach, pumpkin seeds, and dark chocolate, and pair iron‑rich meals with vitamin C to improve uptake. Hydration is critical – aim for at least 2 L of water a day, because dehydration can mask the benefits of micronutrients. Light aerobic activity, such as a 30‑minute walk, improves circulation and encourages the delivery of nutrients to brain tissue. Keep a detailed headache diary that records pain intensity, duration, food intake, supplement timing, sleep quality, and stress levels; this will let you see patterns and assess which interventions are working. Re‑evaluate your blood work after three months and adjust dosages accordingly, always in consultation with your healthcare provider. Finally, remember that supplements are adjuncts, not replacements – a balanced diet rich in whole foods remains the foundation of headache prevention.
Sarah Riley
October 31, 2025 AT 16:32From a pharmacokinetic standpoint, the split‑dose magnesium regimen optimizes bioavailability while minimizing renal clearance, thereby sustaining neuronal membrane stability.
Tammy Sinz
November 2, 2025 AT 04:39Looking at the data, you can see a clear correlation between low vitamin D levels and increased pro‑inflammatory cytokine activity, which directly sensitizes the trigeminal nociceptors. When you boost D‑status, those cytokines drop, reducing peripheral sensitization and ultimately lowering migraine frequency. It’s not just a myth; multiple controlled trials have quantified a 30‑40 % reduction in attack days after normalizing vitamin D. Combine that with adequate magnesium and omega‑3 intake, and you’re targeting both vascular tone and neuroinflammation simultaneously. So the bottom line: a comprehensive micronutrient protocol is essential for anyone serious about headache management.
Christa Wilson
November 3, 2025 AT 16:45Great info, feel better soon! 😊