
Getting the right dose of medicine to a baby isn’t just tricky-it can be life-or-death. One wrong drop, one misread label, one kitchen spoon used as a measuring tool, and you could be facing an emergency room visit. In the U.S. alone, over 50,000 children under five end up in emergency departments every year because of medication errors. And nearly a quarter of those are babies under one year old. The problem isn’t usually bad intentions. It’s confusion. Confusion over concentrations. Confusion over measurements. Confusion over what’s safe.
Why Concentration Matters More Than You Think
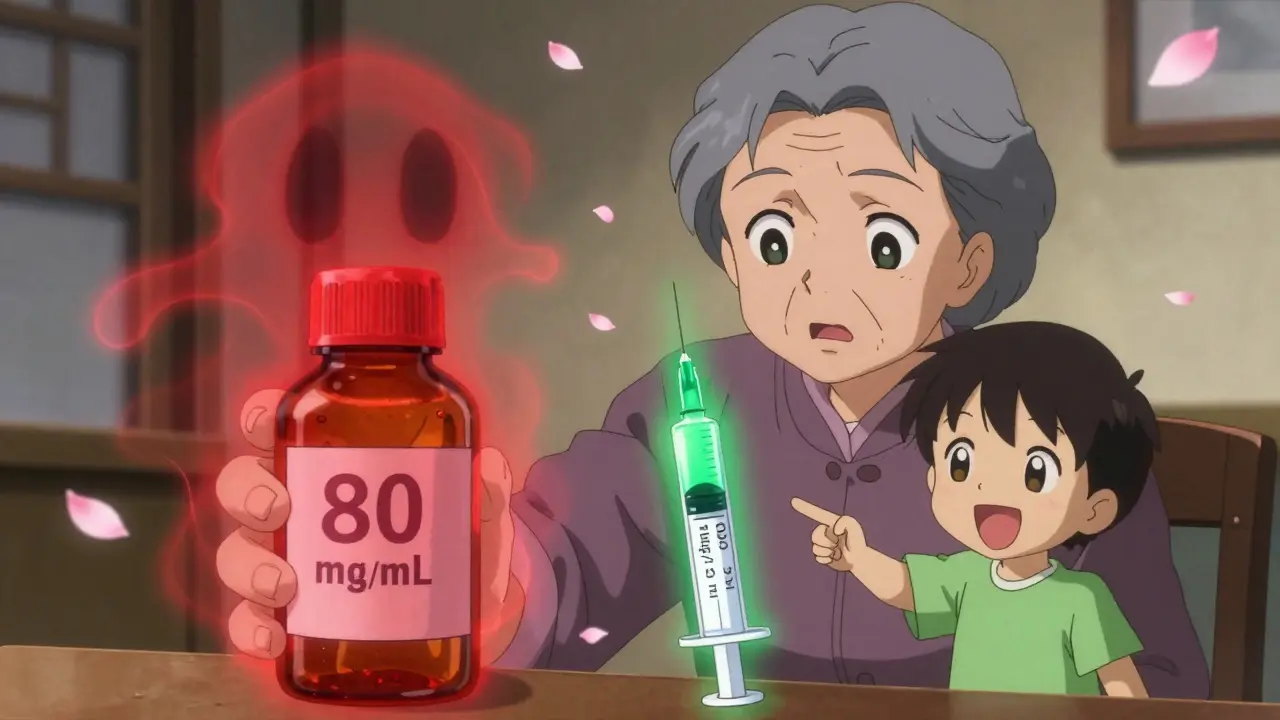
Not all infant medications are made the same. The biggest danger? Mixing up infant and children’s formulas. For years, acetaminophen (the active ingredient in Tylenol) came in two forms: one for babies at 80 mg per mL, and another for older kids at 160 mg per 5 mL. Parents didn’t realize they were giving five times more medicine than intended. That mistake led to hundreds of overdoses. In 2011, the FDA stepped in and made it law: all infant acetaminophen must now be 160 mg per 5 mL. That’s the same concentration as children’s liquid. It sounds simple, but the damage was already done. Many parents still carry old bottles or grab the wrong one off the shelf.Same goes for ibuprofen. Infant drops used to be more concentrated than children’s liquid. Today, both are standardized at 100 mg per 5 mL. But if you’re using an old bottle from a drawer, or your grandma’s medicine cabinet, you could be giving a dangerous dose. Always check the label. Look for the concentration: 160 mg/5 mL for acetaminophen, 100 mg/5 mL for ibuprofen. If it says anything else, don’t use it.
Drops vs. Syringes: The Real Safety Battle
Many infant medications come with a dropper. It looks easy. Squeeze the bulb, fill it up, and drip it in. But here’s the truth: droppers are unreliable. A 2018 study found that 73.6% of parents gave the wrong dose using a dropper. Why? Because drops aren’t consistent. One person’s drop is bigger than another’s. The bottle might be tilted. The bulb might not be squeezed the same way twice.Oral syringes are the gold standard. Not the plastic ones that come with the medicine-those are often too big and imprecise. Use a syringe with 0.1 mL or 0.2 mL markings. These let you measure down to the exact drop. A 2019 study showed that using these syringes cuts dosing errors by 67% compared to medicine cups or droppers. And in a 2020 trial at Cincinnati Children’s Hospital, parents using oral syringes got the dose right 89.3% of the time. Those using cups? Only 62.1%.
Pro tip: Keep a dedicated oral syringe in your diaper bag. Don’t reuse one that’s been used for other things. Clean it after each use with warm water. Store it separately from the medicine bottle. Label it with the child’s name if multiple kids are in the house.
How to Calculate the Right Dose
You can’t just give a baby medicine based on age. Weight matters. Always know your baby’s weight in kilograms. Most pediatricians give this to you at checkups, but if you’re unsure, weigh your baby on a baby scale and convert pounds to kilograms (divide by 2.2).For acetaminophen, the safe dose is 10 to 15 mg per kilogram of body weight, every 4 to 6 hours. Never give more than five doses in 24 hours. For ibuprofen, it’s 5 to 10 mg per kg, every 6 to 8 hours, max four doses a day.
Let’s say your baby weighs 8 kg. For acetaminophen: 8 kg × 10 mg = 80 mg minimum. 8 kg × 15 mg = 120 mg maximum. The concentration is 160 mg per 5 mL. So 80 mg equals 2.5 mL. 120 mg equals 3.75 mL. Use your oral syringe to measure exactly that. Don’t round up. Don’t guess. If the number is messy-like 3.75 mL-use the syringe’s fine markings. That’s why they’re there.
Use a dosing calculator if you’re unsure. The National Poison Control Center’s Help Me Choose tool (at poison.org) walks you through weight, concentration, and dose. It’s free, reliable, and handles over 14,000 queries a year with near-perfect accuracy.
What Not to Use: Kitchen Spoons and Old Bottles
A teaspoon is not a medicine teaspoon. A tablespoon is not a medicine tablespoon. A kitchen spoon varies wildly. One study found that 43.6% of parents used kitchen spoons to measure liquid meds. And 57.2% of those gave doses that were off by more than 20%. That’s not a little mistake. That’s a risk of overdose.And don’t use old medicine. Even if it’s the same brand, the concentration may have changed. Or the bottle may be expired. Or the cap may not be child-resistant anymore. If it’s been sitting around for months, toss it. Medicines lose potency. And old bottles don’t always have clear labels anymore.
Grandparents are especially at risk. A 2023 study found caregivers over 65 made over three times more dosing errors than parents under 30. Vision problems, outdated knowledge, and memory issues all play a part. If your baby’s grandparent is giving medicine, sit with them. Show them the syringe. Point out the concentration on the label. Walk through the math once. It’s not about trust. It’s about safety.
The Five-Step Safety Checklist
The American Academy of Pediatrics recommends this simple five-step process every time you give medicine:- Confirm weight: Know your baby’s weight in kilograms. Write it down.
- Calculate dose: Use 10-15 mg/kg for acetaminophen, 5-10 mg/kg for ibuprofen.
- Check concentration: Look at the label. Is it 160 mg/5 mL? 100 mg/5 mL? If not, stop.
- Use the right tool: Oral syringe with 0.1 mL markings. No droppers. No spoons.
- Double-check: Have another adult look at your calculation and the syringe before you give it.
Parents who follow all five steps reduce dosing errors by 82%. That’s not a small number. That’s life-saving.
What About Cold and Cough Medicines?
Skip them. Completely. The FDA has warned since 2008 that over-the-counter cough and cold medicines are not safe for children under 2. In 2021, they reinforced it: no OTC cold medicines for kids under 6. Why? Because they often contain multiple active ingredients-antihistamines, decongestants, cough suppressants. Combine those with acetaminophen or ibuprofen, and you risk overdose. Even a single dose can cause seizures, fast heart rates, or breathing problems.If your baby has a cold, use saline drops and a bulb syringe for the nose. A cool-mist humidifier helps. Honey (only for babies over 12 months) soothes coughs. But don’t give medicine unless a doctor says to.
What’s Changing? Smart Syringes and Color-Coding
The future of infant medication safety is here. In January 2023, the FDA approved the first connected oral syringe-MediSafe SmartSyringe. It pairs with a phone app. You scan the medicine bottle. The app calculates the dose. The syringe won’t release the medicine unless it’s correct. In trials, it was 98.7% accurate.The FDA is also testing color-coded labels: blue for infants, green for children. That way, you can’t grab the wrong bottle by accident. The CDC wants to cut infant dosing errors by half by 2026. They’re pushing for better packaging, clearer labels, and more education.
But none of that matters if you don’t know what to look for. Always read the label. Always measure with a syringe. Always double-check. Your baby’s life depends on it.
When to Call Poison Control
If you’re unsure whether you gave the right dose-if you think you gave too much, too little, or the wrong medicine-call Poison Control immediately. In the U.S., it’s 1-800-222-1222. It’s free, confidential, and available 24/7. Don’t wait for symptoms. Don’t Google it. Call.Most calls are answered in under 30 seconds. They’ve helped prevent over 14,000 emergency visits in 2022 alone. They’re not there to judge. They’re there to help.
Sheryl Dhlamini
January 30, 2026 AT 07:42OMG I just realized I used a kitchen spoon last week when my baby had a fever. I thought it was fine since it was 'a little bit.' Now I'm shaking. Thank you for this post. I'm buying an oral syringe today. No more guessing.
Doug Gray
January 30, 2026 AT 22:41It's ironic, really. We've engineered pills to nanometer precision, yet we still trust parents to eyeball liquid meds with droppers that vary by 40%. Capitalism didn't optimize for safety-it optimized for shelf space and label legibility. The FDA's 'standardization' is just damage control. We need mandatory smart syringes. Not as a luxury. As a baseline.
LOUIS YOUANES
January 31, 2026 AT 22:47Let’s be real-most parents don’t even know what a milligram is. They see ‘160 mg/5 mL’ and think it’s a code for a new iPhone update. I’ve seen moms use baby bottles as measuring tools. No wonder ERs are packed. This isn’t negligence. It’s systemic failure. The system expects parents to be pharmacists while sleep-deprived and crying. That’s not parenting. That’s a trap.
Alex Flores Gomez
February 2, 2026 AT 11:16Oral syringes are the only way. I used to use the dropper that came with the bottle. Then my kid threw up half the dose. Now I use a 1mL syringe with 0.1 marks. I clean it with hot water and vinegar. I label it with sharpie. I keep it in a ziplock in the diaper bag. It’s not hard. It’s just not taught. Schools should teach this. Like, in kindergarten.
Pawan Kumar
February 3, 2026 AT 09:55Did you know the pharmaceutical industry lobbied against color-coded labels? They said it would 'confuse the supply chain.' But the real reason? They make more money selling multiple concentrations. Standardization cuts profits. The FDA doesn't protect you-they protect shareholders. And the 'smart syringe' is just another product they'll charge $50 for. Wake up.