When your stomach hurts, you’re tired all the time, and you’re rushing to the bathroom multiple times a day, it’s easy to assume it’s just a bad stomach bug. But if these symptoms stick around for weeks or months, it might be something deeper - like Crohn’s disease or ulcerative colitis. Both are types of inflammatory bowel disease (IBD), and while they sound similar, they’re not the same condition. Knowing the difference matters - because it changes everything about how you’re treated, what complications to watch for, and even how you manage your diet and daily life.
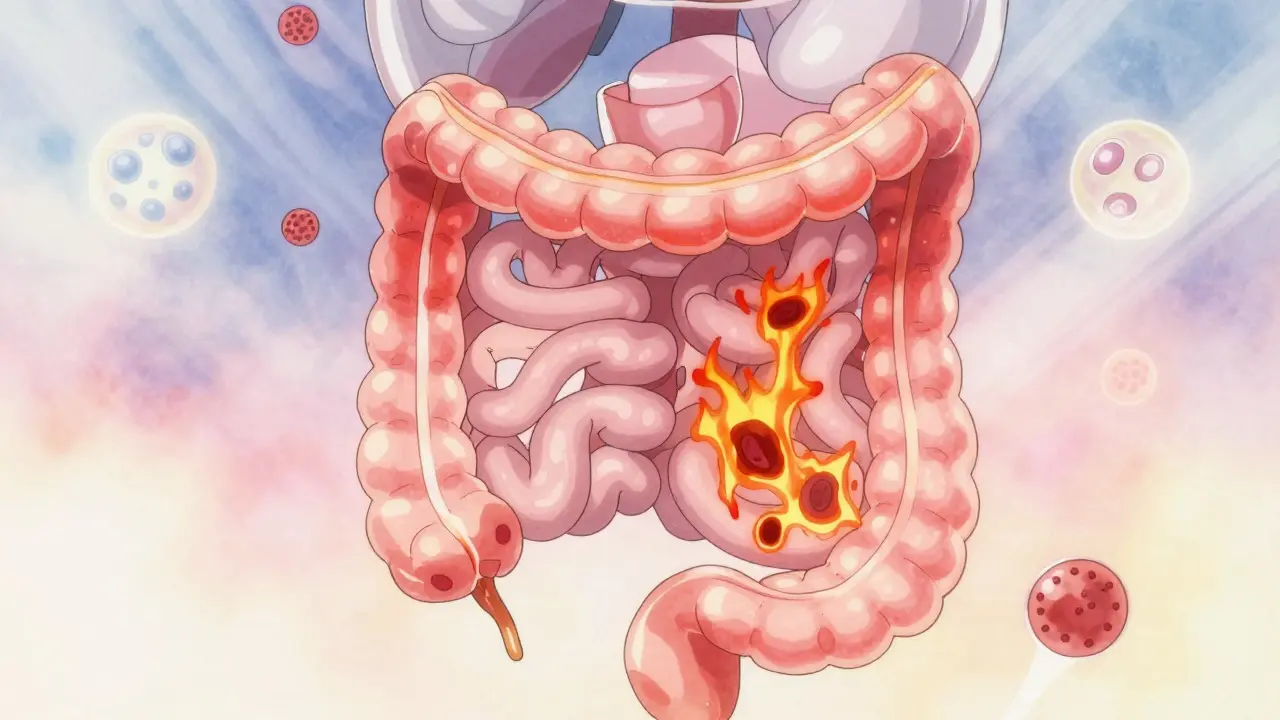
Where the Inflammation Happens
Ulcerative colitis only affects the colon and rectum - the last part of your digestive tract. The inflammation starts at the rectum and moves upward in a continuous line, never skipping a section. It’s like a slow burn along the inner lining of your large intestine. Crohn’s disease is more unpredictable. It can show up anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (the ileum) or the beginning of the colon. But here’s the key: it doesn’t spread evenly. Instead, it creates patches of damage with healthy tissue in between - what doctors call "skip lesions." Think of it like a string of burnt-out light bulbs with working ones in between. This difference isn’t just academic. It affects how doctors test for it. If you’re having symptoms and your colonoscopy shows continuous redness and ulcers starting at the rectum, it’s likely ulcerative colitis. If you see patchy inflammation, deep craters, or cobblestoning (a bumpy, uneven surface), it points to Crohn’s.How Deep Does the Damage Go?
Ulcerative colitis stays shallow. It only affects the innermost layer of the bowel wall - the mucosa. That’s why bleeding is so common. The surface is literally breaking down. Crohn’s disease goes deeper. It can eat through all layers of the intestinal wall - the mucosa, the muscle, even the outer covering. This is why Crohn’s leads to complications like fistulas (tunnels between organs) and strictures (narrowing from scar tissue). These don’t happen in ulcerative colitis because the inflammation doesn’t reach deep enough. A 2022 study in the Journal of Crohn’s and Colitis found that 85% of people with Crohn’s showed transmural inflammation on endoscopic ultrasound - meaning the damage went all the way through. In ulcerative colitis? Zero percent.What Complications Can You Expect?
Because of where and how deeply they attack, these diseases lead to very different risks. With Crohn’s, about 1 in 3 people will develop a stricture over their lifetime. About 1 in 4 will get a fistula - an abnormal connection between the bowel and another organ, like the bladder or skin. These can cause infections, abscesses, or even require multiple surgeries. Ulcerative colitis doesn’t usually cause fistulas or strictures. But it has its own scary complication: toxic megacolon. This is when the colon suddenly swells and loses its ability to contract. It’s rare - happening in only about 5% of UC cases - but it’s life-threatening and needs emergency treatment. Both conditions can also cause problems outside the gut. Joint pain, skin rashes like erythema nodosum, and eye inflammation are common in both. But one condition has a strong link to liver disease: primary sclerosing cholangitis (PSC). Around 5% of people with ulcerative colitis develop PSC. Only about 1% of Crohn’s patients do.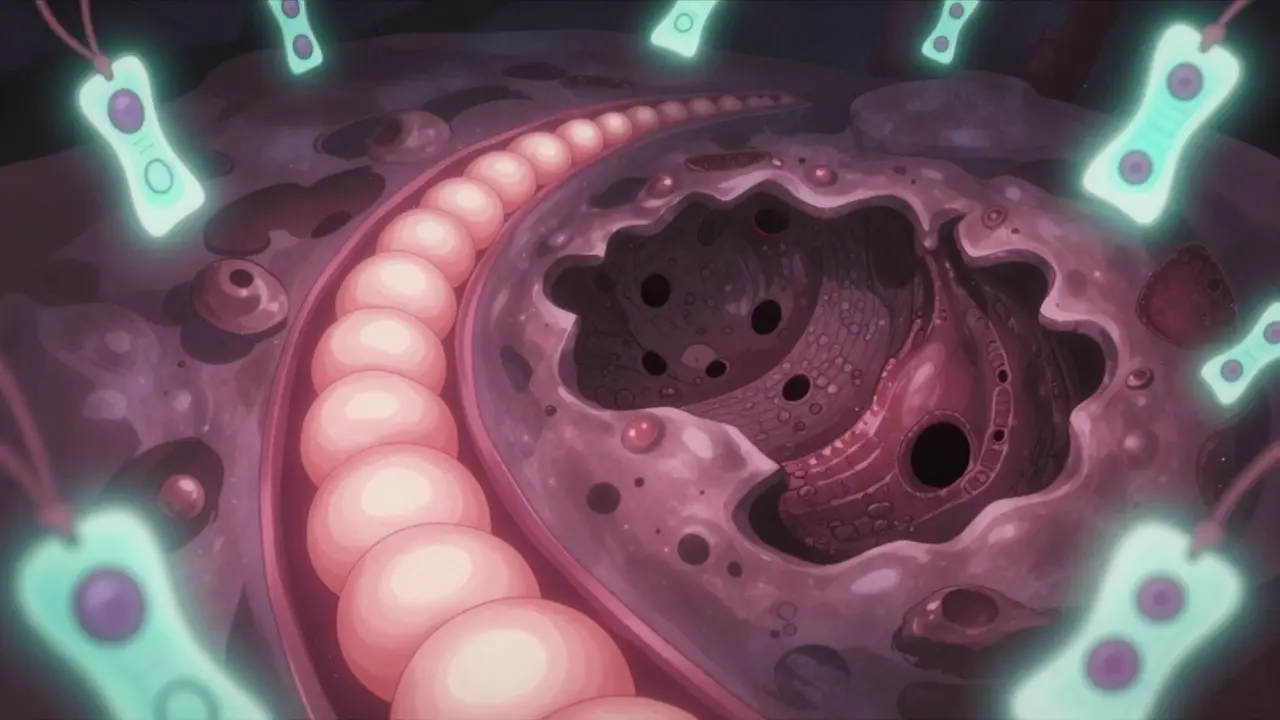
How Doctors Tell Them Apart
There’s no single blood test that says "Crohn’s" or "UC." Diagnosis is a puzzle made of clues. Colonoscopy with biopsy is the gold standard. In ulcerative colitis, you’ll see uniform inflammation, tiny ulcers, and sometimes pseudopolyps - bumps of healing tissue. In Crohn’s, you’ll see skip areas, deep ulcers, and granulomas (tiny clusters of immune cells) - which appear in about 30% of Crohn’s cases but never in UC. Blood tests help too. About 60-70% of ulcerative colitis patients test positive for pANCA (a type of antibody). Only 10-15% of Crohn’s patients do. Fecal calprotectin (a protein that signals gut inflammation) is high in both, but tends to be higher in UC. Imaging is critical for Crohn’s. A capsule endoscopy (a pill-sized camera you swallow) finds small bowel damage in 70% of suspected Crohn’s cases that look normal on colonoscopy. MRI enterography shows fistulas and deep inflammation with 85% accuracy. Still, about 10-15% of cases start out as "indeterminate colitis" - where doctors can’t tell which one it is. Sometimes, it takes years and more symptoms before the diagnosis becomes clear.Treatment Differences
Both conditions use anti-inflammatories, immunosuppressants, and biologics. But the approach isn’t the same. For mild to moderate ulcerative colitis, doctors often start with 5-ASAs - drugs like mesalamine - delivered as enemas or suppositories. These put the medicine right where it’s needed. About 60-80% of patients go into remission with this method. Crohn’s disease usually needs systemic treatment because it’s not just in the colon. Oral or injected drugs like azathioprine or biologics (infliximab, adalimumab) are more common. The SONIC trial showed azathioprine helped 40-50% of Crohn’s patients reach remission in 17 weeks. Biologics work better for Crohn’s than UC. In the GEMINI trials, anti-TNF drugs led to remission in 30-40% of Crohn’s patients after 54 weeks, compared to 20-30% for UC. Surgery is a big difference. For ulcerative colitis, removing the entire colon and rectum is a cure. Many patients get an ileal pouch - a new internal reservoir made from the small intestine - so they can still go to the bathroom normally. About 10-15% of UC patients end up with this surgery within 10 years. For Crohn’s, surgery is not a cure. Surgeons remove the damaged section, but the disease almost always comes back - often right next to the surgical site. Half of Crohn’s patients need another operation within 10 years.
What Patients Actually Experience
Real-life symptoms vary too. People with ulcerative colitis often describe urgent, frequent bowel movements - sometimes 10 or more a day - and bright red blood in the stool. It’s hard to miss. A 2023 survey of 1,200 IBD patients found 87% of UC patients reported urgency, compared to 68% of Crohn’s patients. Rectal bleeding was reported by 75% of UC patients, but only 35% of Crohn’s patients. Crohn’s patients more often struggle with malnutrition. Because the small intestine is often involved, nutrients like vitamin B12, iron, and fat-soluble vitamins don’t get absorbed well. About 65% of Crohn’s patients report weight loss or dietary challenges, compared to 30% of UC patients. Trigger patterns differ too. On Reddit’s r/IBD community, UC patients most often blame stress - cited in 62% of flare discussions. Crohn’s patients point to food: dairy in 45%, high-fiber foods in 38%.What’s New in Treatment?
The future of IBD care is getting more targeted. Fecal microbiota transplantation (FMT) - basically, a poop transplant - showed 32% remission rates in ulcerative colitis in the VERSUTIL trial. For Crohn’s? Only 22%. New drugs are on the horizon. Etrolizumab is being tested for UC, and mirikizumab for Crohn’s. Both are biologics that target specific immune pathways, and FDA decisions are expected by late 2024. Costs are rising. In the U.S., severe Crohn’s averages $38,451 per year in medical costs. Severe UC is slightly lower at $31,789 - but still a huge burden.What You Should Know
If you’ve been diagnosed with IBD, don’t just accept the label. Ask: Is this Crohn’s or ulcerative colitis? Because the answer changes your treatment plan, your risk of complications, and your long-term outlook. Even if it’s unclear at first - "indeterminate colitis" - keep tracking your symptoms. Over time, the pattern will emerge. Neither condition is curable - except for ulcerative colitis, where removing the colon is a cure. But both are manageable. With the right diagnosis, the right treatment, and the right support, people with IBD live full, active lives.Can you have both Crohn’s disease and ulcerative colitis at the same time?
No, you can’t have both at the same time. They’re two distinct conditions with different patterns of inflammation. But sometimes, especially early on, doctors can’t tell which one you have - this is called "indeterminate colitis." About 10-15% of IBD cases start this way. Over time, as symptoms and test results develop, most cases get reclassified as either Crohn’s or ulcerative colitis.
Does diet cause IBD?
No, diet doesn’t cause Crohn’s disease or ulcerative colitis. These are autoimmune conditions triggered by a mix of genetics, immune system dysfunction, and environmental factors like antibiotics or smoking. But food can make symptoms worse. People with Crohn’s often react to high-fiber or fatty foods, while UC patients may find dairy or spicy meals trigger flares. Eating well helps manage symptoms - but it won’t prevent or cure IBD.
Is IBD the same as IBS?
No. IBS (Irritable Bowel Syndrome) is a functional disorder - meaning the gut looks normal but doesn’t work right. It causes cramping, bloating, and changes in bowel habits, but no inflammation or tissue damage. IBD (Crohn’s and ulcerative colitis) involves actual inflammation, ulcers, and sometimes permanent damage. IBS is common and not life-threatening. IBD is serious and requires medical treatment.
Can IBD turn into cancer?
Yes, long-standing ulcerative colitis increases the risk of colon cancer, especially if the entire colon is affected for more than 8-10 years. Regular colonoscopies with biopsies are recommended to catch precancerous changes early. Crohn’s disease also raises cancer risk slightly, particularly in the small intestine or if there’s chronic inflammation. Surveillance is key for both.
Will I need surgery?
For ulcerative colitis, surgery is an option - and can be curative. About 10-15% of patients have their colon removed within 10 years. For Crohn’s, surgery is common - about half of patients need a resection within 10 years - but it’s not a cure. The disease often returns near the surgical site. Surgery is usually done when medications fail or complications like strictures or fistulas develop.
Katrina Morris
January 6, 2026 AT 16:24Just wanted to say this post saved me months of googling. I was diagnosed with "indeterminate colitis" last year and honestly felt lost. Now I understand why my doctor keeps pushing for repeat scopes. It’s not that they don’t know - they’re waiting for the pattern to reveal itself. Thank you for laying this out so clearly.
Also, the part about FMT being more effective for UC? That’s wild. I’m on a waiting list for a transplant and honestly didn’t expect it to be this targeted.
Stay healthy, everyone.
Rachel Steward
January 8, 2026 AT 13:24Let’s be real - the entire medical establishment is just guessing. They call it "indeterminate colitis" because they don’t have the guts to say they’re clueless. Biologics cost a fortune and half the time they don’t work. They’re just buying time while the system profits. And don’t get me started on the "pseudopolyps" - that’s just fancy language for "healing wounds they can’t fix."
Real cure? Remove the colon and be done with it. But no, they’d rather keep you on drugs for life. Wake up.
Vince Nairn
January 8, 2026 AT 18:55So I read this whole thing while on the toilet (yes, again) and I’m just here to say… wow. I’ve had Crohn’s for 12 years and no one’s ever explained skip lesions like burnt-out lightbulbs. That’s now my new mental model.
Also, the fact that UC can be cured by removing the colon but Crohn’s can’t? That’s brutal. I’m not mad - I’m just… deeply sad. And also, thank you for not sugarcoating the surgery stats.
Kyle King
January 9, 2026 AT 14:58Anyone else notice how every single study cited here was funded by Big Pharma? Of course they say biologics work better for Crohn’s - they make billions off them. The real answer is fasting, turmeric, and avoiding gluten. But you won’t hear that from a GI who gets paid per infusion.
They’re not treating you. They’re monetizing your pain.
Christine Joy Chicano
January 11, 2026 AT 04:57I’ve been living with UC for eight years and I’ve never seen someone articulate the difference between mucosal and transmural inflammation so vividly. The "burnt-out lightbulb" analogy for Crohn’s skip lesions? Genius. And the PSC link to UC? I didn’t know that until now - my liver enzymes have been weird for years. I’m scheduling a hepatology consult tomorrow.
Also, the part about 5-ASAs being delivered via enema? That’s the secret weapon. I thought I was being weird for using the suppositories in public restrooms. Turns out, I’m just doing it right.
Mina Murray
January 12, 2026 AT 07:50They say you can’t have both Crohn’s and UC. Bullshit. I had both. Or at least, I had the symptoms of both. My doctor called it "indeterminate" because he didn’t want to admit he was wrong. I got a second opinion - and guess what? The second doc said I had Crohn’s with colonic involvement. Then the third said it was UC with patchy inflammation. I stopped going to doctors after that.
Just eat clean. Avoid dairy. Sleep. That’s all you need.
Adam Gainski
January 13, 2026 AT 18:17This is one of the clearest breakdowns I’ve ever read on IBD. I’m a nurse and I’ve worked with dozens of IBD patients - but I still learned something. The stats on fistulas vs. toxic megacolon? Perfect. The FMT numbers? Eye-opening.
One thing I’d add: don’t underestimate the role of vitamin D. Low levels are rampant in both conditions and correlate with flare frequency. I’ve seen patients stabilize just by hitting 50-70 ng/mL. It’s not a cure, but it’s a quiet hero.
Elen Pihlap
January 15, 2026 AT 06:13i just want to know why i keep getting diarrhea after eating pizza
Ayodeji Williams
January 16, 2026 AT 07:52bro this post is fire 🔥 but u know what’s worse? doctors telling u it’s stress then u find out it’s crohn’s 2 years later 😭 i lost my job because they thought i was faking it. now i’m on adalimumab and still can’t afford rent. why is healthcare like this?? 🤡
Anthony Capunong
January 18, 2026 AT 02:37Look, I’ve read this whole thing and I’m just gonna say it - America’s medical system is broken. Why are we paying $38k a year for Crohn’s treatment while other countries give people biologics for free? This isn’t science. This is capitalism with a stethoscope. If you’re not American, you’re lucky. If you are? You’re being exploited.
Paul Mason
January 18, 2026 AT 06:32My mum had UC and got her colon out in '98. She said it was the best decision she ever made. No more meds, no more panic attacks before leaving the house. She lives in Spain now - healthcare’s cheaper there, and she’s never looked back.
Don’t be scared of surgery. It’s not the end. It’s the beginning of living again.
Kamlesh Chauhan
January 19, 2026 AT 08:20who cares about all this medical jargon
just stop eating bread and youll feel better
my cousin did it and now he runs marathons
its all in your head anyway
stop being weak
Emma Addison Thomas
January 20, 2026 AT 06:01Thank you for writing this with such care. I’m from the UK and I’ve seen how little awareness there is here - even among GPs. I’ve had to educate my own family about the difference between IBD and IBS. This post will be my go-to link from now on.
One small thing: the mention of PSC and UC - I’ve been diagnosed with both. It’s rare, but it happens. If anyone else has PSC alongside UC, please reach out. We need a support group.
Sai Ganesh
January 21, 2026 AT 10:41As someone from India, I’m shocked no one mentioned Ayurveda here. My uncle used to take Triphala, amla, and turmeric paste daily. His Crohn’s went into remission for 7 years. Modern medicine has its place, but we can’t ignore centuries of traditional knowledge. The West thinks it owns science - but healing is global.