
When you hear "serotonin," you might think of mood, sleep, or that feeling of calm after a good night’s rest. But if you’re taking an antidepressant-or thinking about adding L-tryptophan as a supplement-you need to understand one critical fact: L-tryptophan and many antidepressants work on the same system. And when they overlap, things can get dangerous.
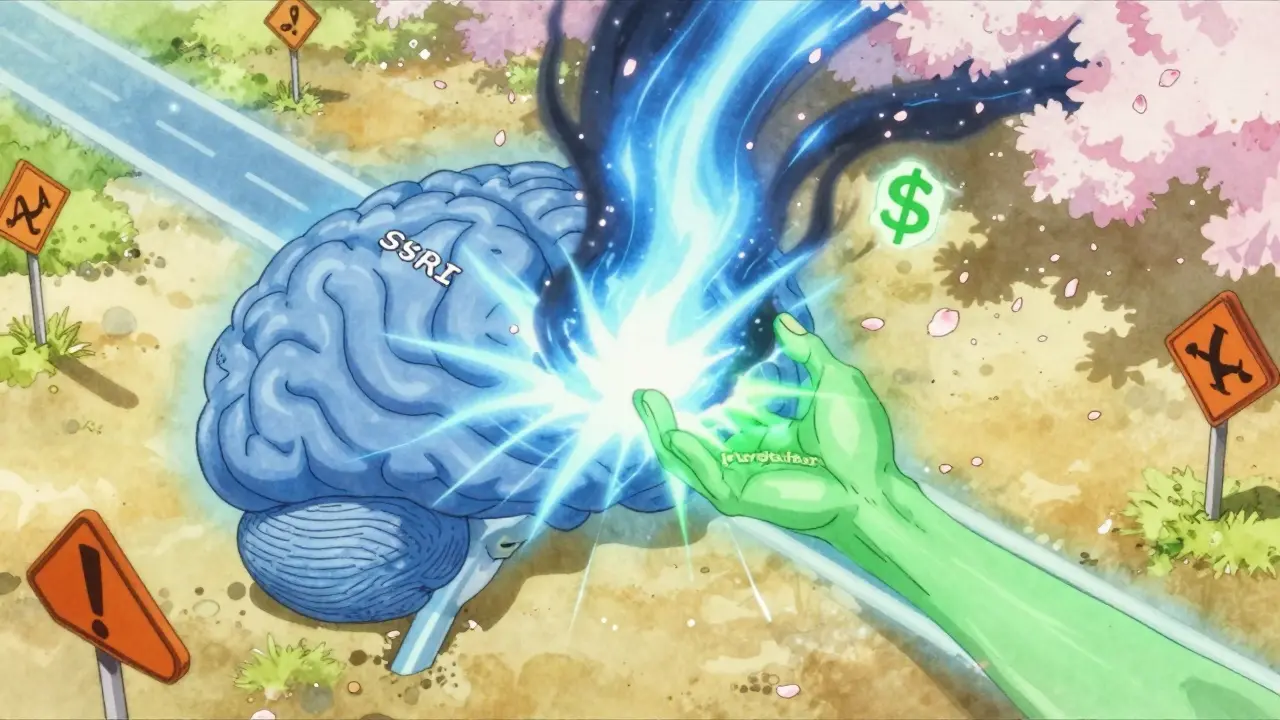
L-tryptophan is an amino acid your body can’t make on its own. It’s the only building block for serotonin. Without it, your brain can’t produce this key neurotransmitter. That’s why it’s sold as a supplement for sleep, mood, and anxiety. But if you’re already on an SSRI like sertraline, fluoxetine, or escitalopram, or an MAOI like phenelzine, combining it with L-tryptophan isn’t just risky-it’s medically warned against by most psychiatrists.
How L-Tryptophan Turns Into Serotonin
Your body doesn’t use L-tryptophan directly as serotonin. It goes through two steps. First, the enzyme tryptophan hydroxylase turns it into 5-hydroxytryptophan (5-HTP). Then, another enzyme, aromatic L-amino acid decarboxylase, converts that into serotonin. This happens almost entirely in the brain. And here’s the catch: the amount of serotonin your brain makes depends almost entirely on how much tryptophan is floating in your blood.
Studies from the 1990s, like the one by Delgado et al. in 1990, showed that when researchers lowered plasma tryptophan levels by 95% using a special amino acid mix, serotonin production in the brain dropped by the same amount. That’s not a small effect-it’s a near-total shutdown. This method, called rapid tryptophan depletion (RTD), is used in labs to test how sensitive someone’s mood is to serotonin changes.
That’s why some people feel worse after skipping a meal, fasting, or eating a high-carb, low-protein diet. Carbs spike insulin, which clears competing amino acids from the blood, letting more tryptophan cross into the brain. But if you’re already on medication that boosts serotonin, adding extra tryptophan can push you over the edge.
Antidepressants and the Serotonin Trap
Not all antidepressants work the same way. SSRIs block the reuptake of serotonin, so more of it stays in the space between brain cells. MAOIs stop the enzyme that breaks down serotonin, so it builds up. Both increase serotonin activity. That’s why they work for depression.
But here’s the problem: when you add L-tryptophan to the mix, you’re not just helping. You’re flooding the system. In a 2022 review of 17 studies involving over 116,000 people, researcher Joanna Moncrieff found no solid proof that depression is caused by low serotonin. But that doesn’t mean serotonin doesn’t matter. It means the story is more complex. What we do know is this: if your brain is already flooded with serotonin from an SSRI, and you add a supplement that makes even more, you’re asking for trouble.
Studies show that 47% of people on SSRIs who undergo tryptophan depletion relapse into depression within hours. That’s not a fluke. It proves that their mood is tightly tied to serotonin levels. But if you take extra tryptophan while on those same drugs? You’re not helping your mood-you’re increasing the risk of serotonin syndrome.
Serotonin Syndrome: The Silent Danger
Serotonin syndrome isn’t a myth. It’s real, it’s dangerous, and it’s happening more often than you think. Symptoms include agitation, confusion, rapid heart rate, high blood pressure, muscle rigidity, sweating, shivering, and in severe cases, seizures or death.
The FDA banned L-tryptophan supplements in 1989 after 1,500 people in the U.S. got eosinophilia-myalgia syndrome (EMS)-a rare, sometimes fatal illness-linked to a contaminated batch. That ban lasted until 2005. Even now, the risk isn’t just about contamination. It’s about combining supplements with prescription drugs.
A 2023 analysis of 1,200 Amazon reviews of L-tryptophan supplements found that 15% of users mentioned serotonin syndrome as a concern. That’s not paranoia. It’s experience. Clinicians on Sermo, a network of over 1.5 million doctors, report that 73% of psychiatrists avoid recommending L-tryptophan to anyone on an SSRI or MAOI. Why? Because the interaction is unpredictable. One person might feel fine. Another might end up in the ER.
What About Other Antidepressants?
Not all antidepressants are created equal. Tricyclics like amitriptyline and desipramine also affect serotonin, but differently. Studies from the 1980s showed they enhance the body’s response to tryptophan. But drugs like bupropion (Wellbutrin) work on dopamine and norepinephrine, not serotonin. People on bupropion don’t relapse during tryptophan depletion. That’s why some doctors consider bupropion a safer option if you’re thinking about trying supplements.
But even then, caution is key. There’s no such thing as a "safe" combo without medical supervision. The American Psychiatric Association’s 2020 guidelines say that if you’re considering L-tryptophan for augmentation (adding it to an existing antidepressant), you need a 7-10 day washout period first. And you need blood tests to monitor tryptophan levels. The therapeutic range? 80-120 μmol/L. Go above that, and you’re in danger.
Who Might Benefit? (And Who Should Stay Away)
Some people with treatment-resistant depression-those who haven’t responded to two or more antidepressants-might see a small benefit from L-tryptophan augmentation. A 2018 study in the Journal of Clinical Psychiatry found a 63% success rate when 3g/day was added to an SSRI for partial responders. But that’s not a recommendation. It’s a research finding. And even then, it required strict monitoring.
On the flip side, if you’re on any serotonergic drug, you should avoid L-tryptophan. That includes:
- SSRIs (Prozac, Zoloft, Lexapro, etc.)
- SNRIs (Effexor, Cymbalta)
- MAOIs (Nardil, Parnate)
- Tricyclics (Amitriptyline, Clomipramine)
- Mirtazapine (Remeron)
- Tramadol, dextromethorphan, St. John’s Wort
Even over-the-counter cough syrups can interact. And if you’re pregnant, have liver disease, or take blood pressure meds? The risks multiply.

The Bigger Picture: Serotonin Isn’t the Whole Story
Here’s the twist: serotonin might not even be the main player in depression. New research since 2020 shows that the kynurenine pathway-what your body does with tryptophan when it doesn’t turn it into serotonin-might be more important. High levels of kynurenine metabolites correlate more strongly with depression severity than serotonin levels do. That means your body might be shunting tryptophan away from mood regulation and into inflammation. So even if you take L-tryptophan, it might not help if your body is stuck in a different metabolic path.
This is why the NIH cut serotonin-focused research funding by 32% in 2023. The field is shifting. Supplements like L-tryptophan are being marketed as mood boosters, but science is moving past the simple "low serotonin = depression" model.
Real-World Advice: What to Do
If you’re not on an antidepressant and you’re considering L-tryptophan for sleep or mild mood support:
- Start low: 250-500 mg at night
- Don’t take it with carbs or alcohol
- Watch for nausea, dizziness, or headaches
- Stop immediately if you feel unusually anxious or agitated
If you’re on an antidepressant:
- Don’t take L-tryptophan without talking to your doctor
- Even "natural" doesn’t mean safe
- Many supplement labels don’t warn about serotonin syndrome-FDA found 41% of products in 2021 lacked proper warnings
- Your pharmacist is a better first stop than Google
The truth? L-tryptophan isn’t the miracle cure it’s sold as. And for people on antidepressants, it’s not worth the risk. The science is clear: when serotonin pathways overlap, the result isn’t better mood-it’s potential harm.
Can I take L-tryptophan with my SSRI for better sleep?
No. Combining L-tryptophan with SSRIs increases the risk of serotonin syndrome, a potentially life-threatening condition. Even if you feel fine, your brain’s serotonin levels could be dangerously elevated. Sleep improvements from L-tryptophan are temporary and outweighed by the risk. Talk to your doctor about safer alternatives like melatonin or cognitive behavioral therapy for insomnia.
Is L-tryptophan better than 5-HTP for depression?
Neither is proven as a standalone treatment for depression. Both are precursors to serotonin, but 5-HTP crosses the blood-brain barrier more easily, making it more potent-and more risky when combined with antidepressants. L-tryptophan requires conversion, which can be blocked by other amino acids. Neither should be used without medical supervision, especially if you’re on any serotonergic medication.
What’s the safe daily dose of L-tryptophan?
The European Food Safety Authority considers up to 5 grams per day safe for healthy adults without medication. But this doesn’t apply to people on antidepressants. For supplementation without drugs, 1-3 grams per day is typical, but effects vary. Always start with 250-500 mg and monitor for side effects. Higher doses increase the risk of nausea, drowsiness, and serotonin-related complications.
Why was L-tryptophan banned in the 1980s?
In 1989, a contaminated batch of L-tryptophan supplements caused eosinophilia-myalgia syndrome (EMS), a rare and sometimes fatal condition that affected over 1,500 people in the U.S. and led to 37 deaths. The FDA banned all L-tryptophan supplements until 2005. While current manufacturing is safer, the risk of interaction with antidepressants remains. The ban wasn’t about the supplement itself-it was about contamination. But the lingering risk of serotonin overload is why many doctors still avoid recommending it.
Do psychiatrists recommend L-tryptophan as an add-on?
It’s rare. A 2022 survey of U.S. psychiatrists found only 29% occasionally recommend it for SSRI partial responders, and even then, only under strict monitoring. In Germany, it’s prescription-approved as Trankimazin, but in the U.S., it’s sold as a supplement with no therapeutic claims. Most clinicians avoid it due to unpredictable interactions and lack of standardized dosing. If you’re considering it, your doctor should run blood tests and require a washout period before starting.