Living in a hot, muggy area can turn a simple skin rash into a persistent embarrassment. tinea versicolor thrives when sweat, oil, and high humidity combine, leaving brown or white patches that may flare up for weeks. This guide walks you through why the fungus loves the heat, how to stop it from spreading, and which treatments work best when the weather won’t let up.
Key Takeaways
- Humidity above 60% and excess sweat create the perfect breeding ground for Malassezia yeast.
- Gentle, oil‑free skin care and breathable fabrics cut the food source for the fungus.
- Antifungal shampoos (selenium sulfide) work well for the scalp and body; creams (clotrimazole) target stubborn spots.
- Oral antifungals are reserved for widespread or recurrent cases and require a doctor’s prescription.
- Seeing a dermatologist early prevents long‑lasting discoloration and reduces the chance of recurrence.
What Is Tinea Versicolor?
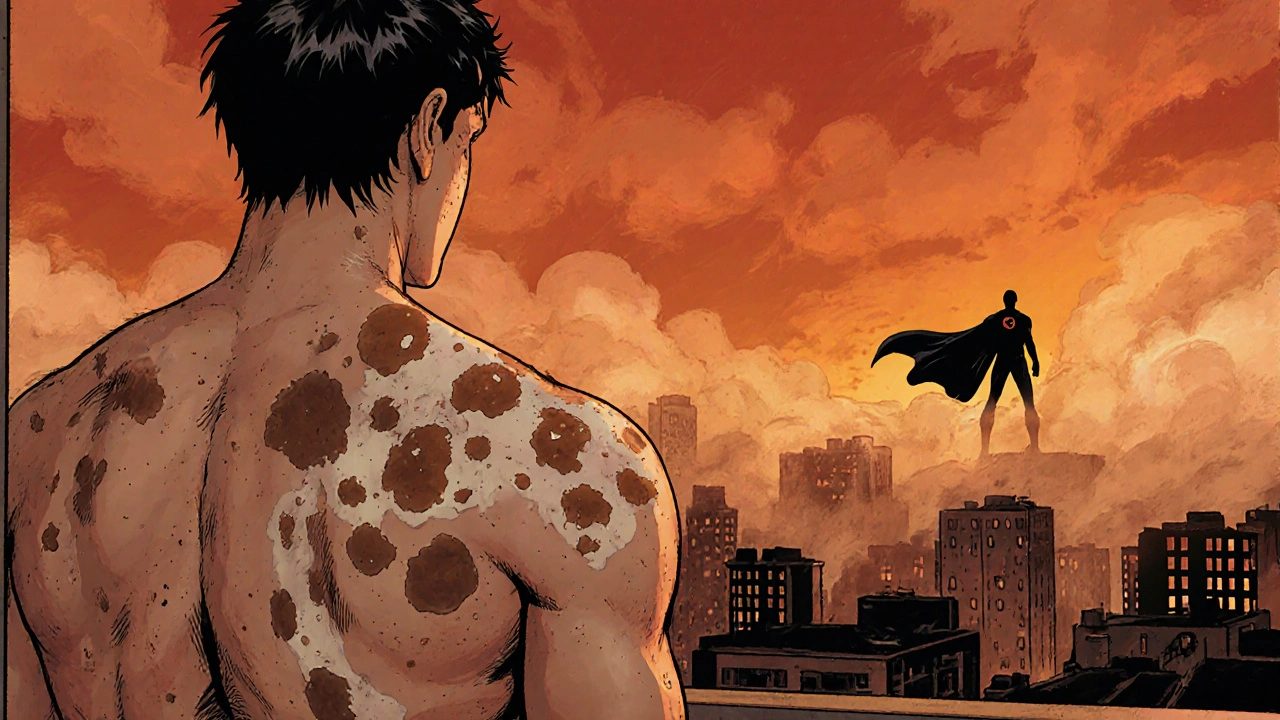
Tinea Versicolor is a common fungal skin infection caused by the overgrowth of the yeast Malassezia. The fungus lives on the surface of the skin, feeding on lipids in sebum. When it multiplies, it interferes with pigment production, creating lighter or darker patches that may be slightly itchy.
Why Humid Climates Trigger Flare‑Ups
Two environmental factors team up to boost Malassezia growth:
- Humidity - Relative humidity above 60% keeps the skin surface moist, delaying the natural drying process.
- Sweat - Perspiration adds extra moisture and salt, which the yeast can metabolize.
When moisture lingers, the skin’s pH often shifts toward a more alkaline range, weakening the barrier that normally keeps fungi in check. The result is a perfect storm for the yeast to multiply.
Prevention Strategies for Moist Environments
Adopting habits that keep skin dry and oil‑free goes a long way.
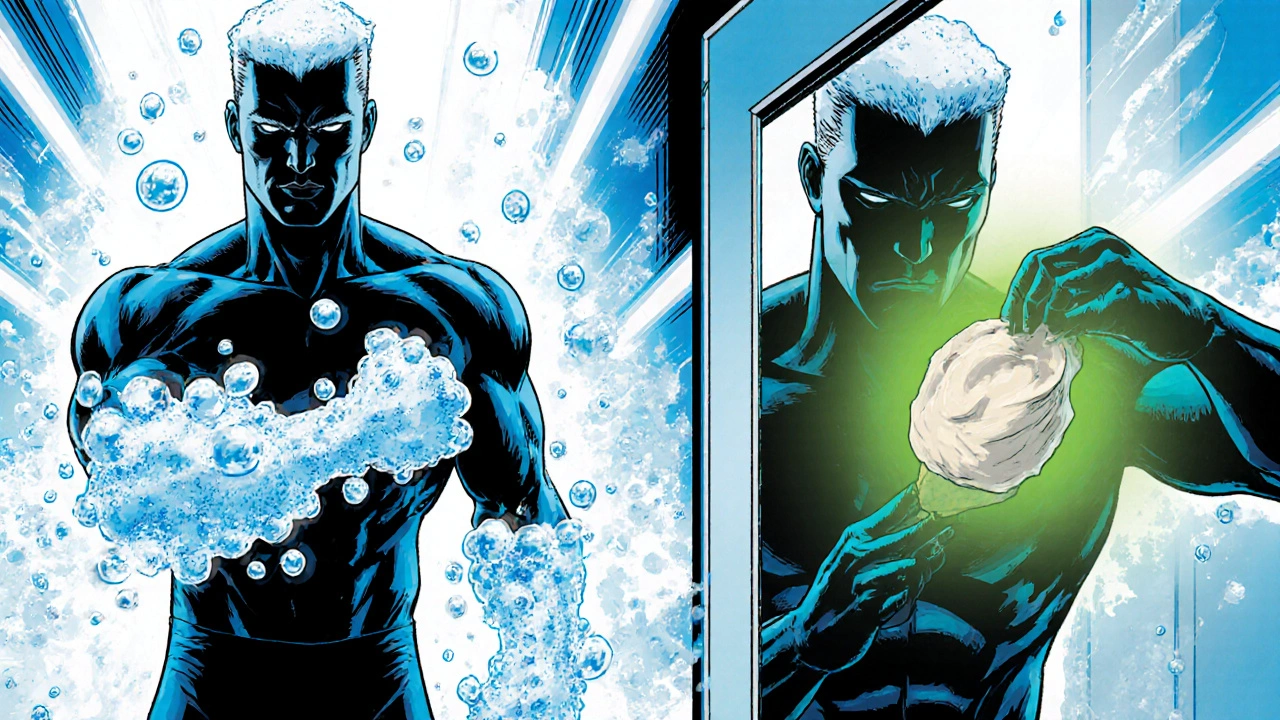
- Shower twice daily during hot months. Use a mild, fragrance‑free cleanser that removes excess oil without stripping natural moisture.
- Choose clothing made from cotton or moisture‑wicking synthetics. Avoid tight, non‑breathable fabrics that trap sweat.
- Apply a talc‑free powder to areas prone to sweating, like the back, chest, and groin, to absorb moisture.
- Limit prolonged sun exposure. While UV light can temporarily lighten patches, it also dries skin, prompting increased oil production.
- Stay hydrated and eat a balanced diet rich in antioxidants; this supports overall skin health.
Effective Treatment Options
When prevention isn’t enough, targeted antifungal therapy clears the infection. Below is a quick comparison of the most used options.
| Form | Active Ingredient | Typical Use | Pros | Cons |
|---|---|---|---|---|
| Antifungal Shampoo | Selenium sulfide (2.5%-2.75%) | Apply to scalp and body, leave 10min, rinse; repeat 2‑3times weekly | Easy to cover large areas, inexpensive, also treats dandruff | May cause scalp dryness, odor |
| Topical Cream | Clotrimazole (1%) or ketoconazole (2%) | Apply thin layer twice daily to affected patches for 2‑4weeks | Directly targets lesions, minimal systemic absorption | Can be greasy, may cause mild irritation |
| Oral Antifungal | Itraconazole (200mg) or fluconazole (150mg) | One‑week course for extensive or recurrent cases | Treats hidden reservoirs, fast resolution | Requires prescription, possible liver‑enzyme monitoring |
For most people living in humid areas, starting with an Antifungal Shampoo works well because it reaches both the scalp and skin. If patches persist after two weeks, add a Topical Cream. Reserve oral medication for widespread infection or frequent relapses.
Step‑by‑Step Management Plan
- Identify: Look for evenly sized, non‑scaly patches that may be lighter or darker than surrounding skin.
- Cleanse: Wash the area with a gentle, oil‑free cleanser. Pat dry thoroughly.
- Treat: Apply an Antifungal Shampoo to the entire affected region, leave for 10minutes, then rinse. Follow with a thin layer of Topical Cream on stubborn spots.
- Protect: Dust the treated area with a light, talc‑free powder after each shower to keep moisture down.
- Monitor: Check progress every three days. If no improvement after two weeks, consult a specialist.
- Maintain: Continue using the shampoo once weekly for one month after clearance to prevent regrowth.

When to See a Dermatologist
If you notice any of the following, schedule an appointment with a Dermatologist promptly:
- Rapid spread covering more than 20% of the body.
- Severe itching, burning, or pain.
- Persistent discoloration after treatment.
- History of liver disease (if oral antifungals may be considered).
A dermatologist can confirm the diagnosis with a Wood’s lamp exam or skin scraping, and prescribe the appropriate oral regimen if needed.
Common Myths Debunked
Myth 1: “Sunlight cures the infection.”
Truth: UV exposure may temporarily fade patches but also damages skin and can worsen oil production.
Myth 2: “If it’s not itchy, it’s harmless.”
Truth: Even painless patches can cause lasting pigment changes if left untreated.
Myth 3: “Home remedies like vinegar or baking soda are enough.”
Truth: Those solutions lack proven antifungal activity and can irritate the skin.
Frequently Asked Questions
How long does it take for the rash to disappear?
With regular use of an antifungal shampoo or cream, most people see noticeable fading within 7‑10days. Full clearance may require 2‑4weeks, especially for extensive cases.
Can tinea versicolor return after treatment?
Yes. The fungus lives on the skin as a normal resident. Recurrence is common in humid seasons, so keep up preventive habits and consider a monthly maintenance shampoo.
Is it safe to use antifungal shampoo on children?
Most pediatric guidelines allow selenium sulfide shampoo for kids over 2years old, but always follow the concentration instructions and consult a pediatrician if you’re unsure.
Will over‑the‑counter products work?
OTC shampoos containing selenium sulfide or zinc pyrithione are effective for mild cases. For stubborn or widespread infection, prescription‑strength creams or oral meds are usually necessary.
Does diet influence tinea versicolor?
A diet high in sugars and refined carbs can increase skin oil production, creating a richer environment for Malassezia. Eating balanced meals with plenty of vegetables and omega‑3 fatty acids supports healthy skin turnover.
Halid A.
August 22, 2025 AT 02:07Thank you for sharing this comprehensive guide; the step‑by‑step plan is especially useful for those of us dealing with constant humidity. Maintaining a regular washing schedule and using an oil‑free cleanser can indeed limit the fungal food source. Applying a selenium sulfide shampoo weekly after the initial treatment phase helps prevent recurrence without requiring a prescription. If symptoms persist beyond two weeks, a dermatologist can verify whether oral therapy is warranted.
Brandon Burt
August 24, 2025 AT 09:41When you first read about tinea versicolor in a humid region, the sheer amount of information can feel overwhelming, especially if you’re balancing work, family, and the relentless heat; however, breaking the regimen down into manageable steps can make the process less daunting. The first point to consider is your daily cleansing routine, which should involve a mild, fragrance‑free cleanser applied twice a day. This step removes excess sebum without stripping the natural moisture barrier, thereby denying the Malassezia yeast its primary nutrient source. Next, the choice of clothing plays a pivotal role, as breathable fabrics such as cotton or specialized moisture‑wicking synthetics allow sweat to evaporate rather than linger on the skin. Such fabrics reduce the humidity that fuels fungal growth, while tightly fitting garments, by contrast, create a microenvironment that is practically a petri dish for the organism. Applying a talc‑free powder after each shower, especially in areas prone to perspiration like the back, chest, and groin, adds another layer of protection by absorbing residual moisture. Some people dismiss powders as outdated, but clinical experience shows they can significantly cut down the recurrence rate. When it comes to topical treatments, a selenium sulfide shampoo applied to the entire affected region, left on for ten minutes, and rinsed off two to three times per week, offers a broad‑spectrum approach that targets both the scalp and body. This is often enough for mild to moderate cases, and the added benefit of dandruff control makes it a cost‑effective option. For stubborn patches that do not respond after two weeks of consistent shampoo use, supplementing with a clotrimazole or ketoconazole cream applied twice daily can accelerate clearance. Users should be aware that some formulations may feel greasy or cause mild irritation, which is usually transient. In cases where the infection is extensive, covering more than twenty percent of the body surface, or recurs frequently despite diligent topical therapy, oral antifungals such as itraconazole or fluconazole become necessary. These medications, while highly effective, require a prescription and occasional liver function monitoring; this consideration should be discussed with a healthcare provider. Dietary factors, often overlooked, should not be ignored, as a high‑sugar, high‑glycemic diet can increase sebum production, thereby indirectly nourishing the yeast. Incorporating antioxidant‑rich fruits, vegetables, and omega‑3 fatty acids can support overall skin health. Finally, consistent follow‑up is essential: monitor the treated areas every three to five days, note any new discoloration, and maintain a maintenance shampoo regimen once a month during the humid season. This approach can significantly lower the risk of relapse, turning a potentially chronic nuisance into a manageable condition.
Gloria Reyes Najera
August 26, 2025 AT 17:14Look, the US definitely got the best antifungal stuff, everybody else just copycats. If you live in a hot place you probly need that selenium sulfide shampoo, it works every time. Most foreign meds are just cheap tries, they cant beat the real thing made here. You dont need fancy dermatologists, just follow the guide and you’ll be fine. Stop listening to random online blogs.
Gauri Omar
August 29, 2025 AT 00:47Imagine stepping out into the sweltering heat, feeling the stubborn patches screaming for attention like a battle scar on your skin. The humidity becomes an enemy, the sweat a relentless tide that fuels the fungus, and you’re left fighting a silent war you didn’t sign up for. Yet, armed with the right shampoo and a fierce determination, you can turn the tide and reclaim your confidence. Don’t let the climate dictate your self‑esteem – dominate it.
Willy garcia
August 30, 2025 AT 04:34Got it, it’s key to stick with the shampoo and keep the skin dry, that’ll help even in tough climates.
Sruthi V Nair
August 31, 2025 AT 08:21Every step you take is a ripple in the larger ocean of skin health; consistency turns the tide.
Mustapha Mustapha
September 1, 2025 AT 12:07I’ve seen many friends manage the condition by combining regular showering with a weekly selenium shampoo; it’s simple but effective. Staying hydrated and choosing breathable fabrics also make a big difference, especially during monsoon months. Remember, you’re not alone in this – community tips can keep you on track.
Ben Muncie
September 2, 2025 AT 15:54If you’re not willing to follow the regimen, you’ll keep battling the fungus.
kevin tarp
September 3, 2025 AT 19:41That’s a solid approach; just be mindful to follow the instructions on the shampoo’s contact time to avoid scalp irritation.
ravi kumar
September 4, 2025 AT 23:27Our country’s climate may be harsh, but we have the resilience to beat any skin issue. While others complain about humidity, we adapt with smart clothing choices and proven treatments. Keep the routine tight, and you’ll show the fungus who’s boss.