Dental Local Anesthetic Dosage Calculator
When a dentist numbs a tooth, the goal is simple: make the procedure painless. But even a routine injection can bring about local anesthesia complications if the right steps aren’t followed. Below you’ll get a clear, step‑by‑step roadmap that cuts those risks down to a minimum, whether you’re the clinician planning the work or the patient sitting in the chair.
What Can Go Wrong? Understanding the Common Risks
Local anesthesia is a targeted, reversible loss of sensation applied to teeth, gums, or surrounding tissue. While it’s generally safe, a handful of complications show up more often than you might think:
- Allergic reaction to the anesthetic agent or its vasoconstrictor.
- Excessive bleeding or hematoma when a blood vessel is nicked.
- Nerve injury leading to temporary or, rarely, permanent numbness.
- Systemic toxicity if the maximum safe dose is exceeded.
- Cardiovascular spikes caused by epinephrine in sensitive patients.
Knowing these possibilities upfront lets you put safeguards in place before the needle even touches the gum.
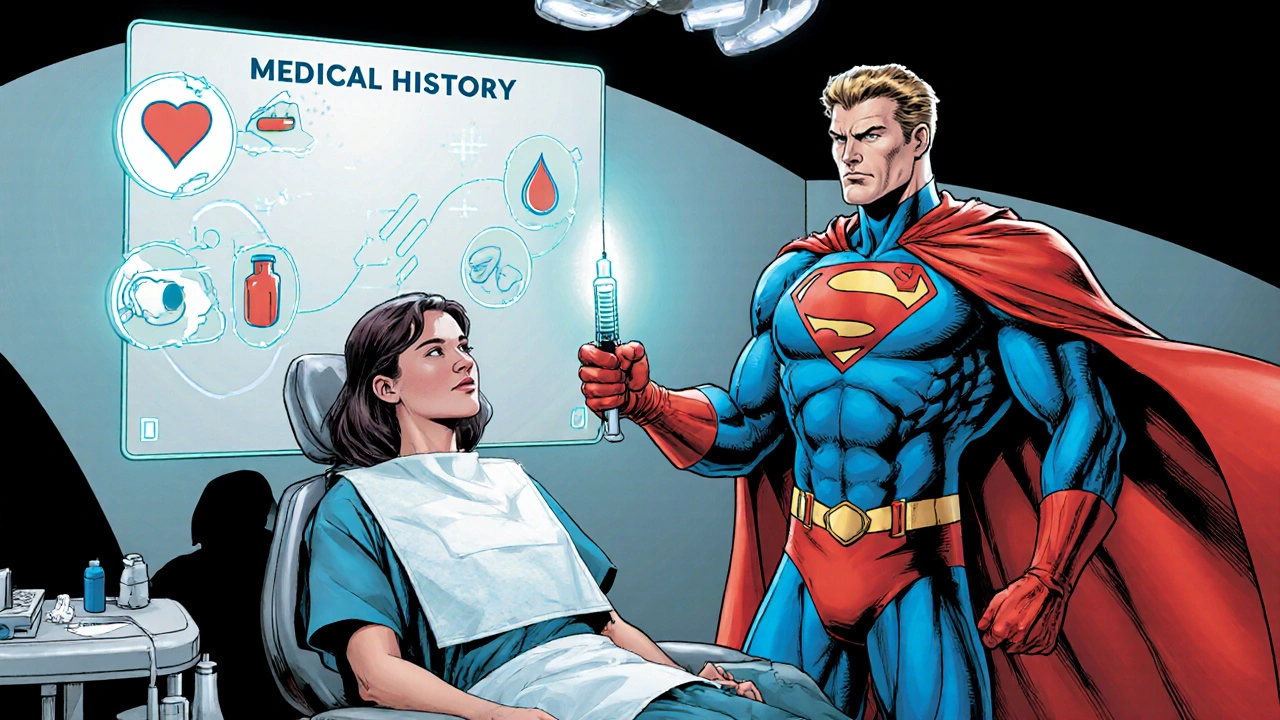
Pre‑Procedure Assessment: The First Line of Defense
Every patient brings a unique medical history. A thorough review can flag red flags early.
- Medical history review: Check for heart disease, hypertension, diabetes, or clotting disorders. These conditions affect how the body handles both the anesthetic and any vasoconstrictor added.
- Medication audit: Beta‑blockers, MAO inhibitors, or anticoagulants can alter drug metabolism or increase bleeding risk.
- Allergy check: Ask explicitly about previous reactions to lidocaine or other local anesthetics. Even a mild rash in the past should raise a flag.
- Informed consent: Document the discussion of risks, benefits, and alternatives. This not only protects the patient legally but also reinforces awareness.
Patient medical history is a collection of health data that guides anesthesia selection and dosing. When you have a solid picture, you can tailor the anesthetic choice and dosage precisely.
Choosing the Right Anesthetic: Matching Drug to Patient
Not all anesthetics are created equal. Each has its own onset speed, duration, and maximum safe dose. Below is a quick comparison of the three most common agents used in dental practice.
| Agent | Onset | Duration (with epinephrine) | Maximum Dose (mg/kg) | Typical Use |
|---|---|---|---|---|
| Lidocaine | 2‑3 minutes | 2‑4 hours | 7 mg/kg | General purpose, most procedures |
| Articaine | 1‑2 minutes | 3‑5 hours | 6.5 mg/kg | Deep infiltrations, surgical extractions |
| Mepivacaine | 2‑3 minutes | 1.5‑3 hours | 6 mg/kg | Procedures where vasoconstrictor should be avoided |
Pick an agent that aligns with the patient’s health status. For someone with cardiovascular concerns, a formulation with a lower epinephrine concentration-or none at all-makes sense. Conversely, a short‑acting drug like lidocaine is a safe bet for quick, simple fillings.
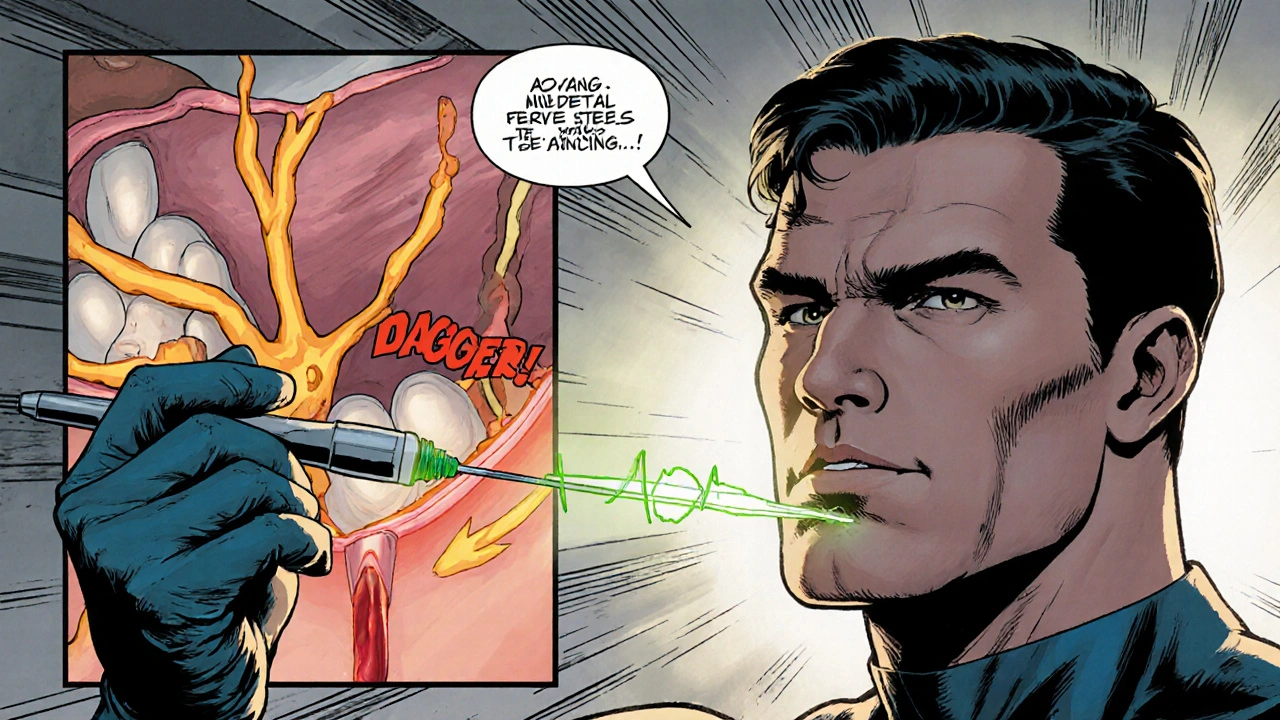
Injection Techniques: Doing It Right the First Time
Even the safest drug can cause trouble if the needle is placed incorrectly.
- Choose the proper gauge: A 27‑gauge needle reduces tissue trauma while still allowing adequate flow.
- Use aspiration: Pulling back on the syringe before injection confirms you’re not inside a blood vessel, preventing systemic absorption of the anesthetic.
- Slow, steady pressure: Depositing the drug over 30‑60 seconds lessens the chance of a sudden spike in blood levels.
- Target anatomical landmarks: Knowing the exact location of the inferior alveolar nerve, mental foramen, or the buccal nerve helps you avoid nerve contact that could cause temporary paresthesia.
The technique itself is a form of injection technique that minimizes tissue trauma and maximizes anesthetic spread. Mastery reduces the odds of nerve injury and hematoma formation.
Managing and Monitoring During the Procedure
Once the area is numb, keep an eye on the patient’s vital signs, especially if epinephrine is part of the mix.
- Pulse oximetry: A fingertip sensor catches early drops in oxygen saturation, which can signal an adverse reaction.
- Blood pressure checks: Hypertensive spikes may occur in anxious patients or those sensitive to vasoconstrictors.
- Observe for signs of toxicity: Dizziness, tinnitus, metallic taste, or blurred vision could indicate the anesthetic has entered the bloodstream in excess.
- Readiness with emergency meds: Have oxygen, an automated defibrillator, and a reversal agent like intralipid on standby for rare systemic toxicity.
Effective monitoring is a continuous assessment that helps catch complications early, allowing quick intervention before a problem escalates.

Post‑Procedure Care: What Patients Should Do After Numbing
Even after the needle’s out, the risk window isn’t closed.
- Ice packs: Apply for 10‑15 minutes to reduce swelling and limit bruising.
- Avoid hot foods for the first hour while numbness persists-burns are a common post‑anesthesia mishap.
- Monitor sensation: If numbness lasts beyond the expected duration, contact the office. Persistent paresthesia may need further evaluation.
- Know the warning signs: Rapid heart rate, severe headache, or swelling at the injection site could signal an allergic reaction or hematoma and warrant immediate medical attention.
Clear discharge instructions empower the patient to spot red flags early and call for help, cutting the chance that a minor issue becomes a major one.
Putting It All Together: A Quick Checklist for Safe Dental Anesthesia
- Review comprehensive patient medical history.
- Confirm no known allergy to lidocaine or articaine.
- Select the anesthetic with the appropriate duration and vasoconstrictor concentration.
- Use a 27‑gauge needle, aspirate before injecting, and inject slowly.
- Monitor vitals throughout, especially if epinephrine is used.
- Provide written post‑procedure care instructions and emergency contact info.
Running through this list each time creates a safety net that catches most pitfalls before they turn into real complications.
Frequently Asked Questions
How long does the numbness from dental local anesthesia usually last?
Typical numbness wears off in 2‑4 hours for lidocaine with epinephrine. Short‑acting agents may fade in as little as 1 hour, while long‑acting drugs like articaine can linger up to 5 hours.
Can I be allergic to the numbing shot?
True allergies to amide anesthetics such as lidocaine are rare, but reactions to preservatives or the vasoconstrictor (epinephrine) do occur. A skin test or prior reaction history helps identify risk.
What should I do if I feel a metallic taste after the injection?
A metallic taste often signals that the anesthetic entered a blood vessel. Sit up, breathe deeply, and alert the dentist immediately. They may need to monitor for signs of toxicity.
Is it safe to have a dental filling if I take blood thinners?
Most dentists can perform routine fillings while you’re on anticoagulants, as long as they use a gentle injection technique and apply proper pressure after the needle is removed. Always discuss dosage with your physician.
Why does my lower lip feel numb for days after an extraction?
Prolonged numbness may indicate temporary nerve irritation, especially if the inferior alveolar nerve was near the injection site. Most cases resolve within a week, but persistent loss of feeling should be evaluated by a dentist or oral surgeon.
Michael Ieradi
September 15, 2025 AT 20:48Reviewing the pre‑procedure checklist is essential for every dental injection. Confirming the patient's weight and any cardiovascular concerns helps set the safe dosage ceiling. Use a 27‑gauge needle and aspirate before depositing the anesthetic. Inject slowly over 30‑60 seconds to avoid a sudden plasma peak. Document the drug choice and dosage in the chart for future reference.
Stephanie Zuidervliet
September 16, 2025 AT 02:22Wow!!! This guide bursts with bullet points, tables, and a calculator, but where's the soul? The relentless list of steps feels like a marching band in a quiet library!!! Yet, the sheer volume almost compensates for the lack of real-life anecdotes!!!
Olivia Crowe
September 16, 2025 AT 07:55Great reminder that a quick allergy check can prevent big setbacks. Keep the needle steady and the patient relaxed, and the numbing goes smoothly!
Aayush Shastri
September 16, 2025 AT 13:28In many Indian clinics we already teach the aspiration technique as a rite of passage for new graduates; it saves nerves and confidence. Adding a simple pulse‑oximeter to the operatory feels like welcoming modern tech into a traditional space. Patients appreciate seeing a monitor, it eases anxiety and shows we care about their vitals. Remember to adjust epinephrine concentration for hypertensive folks, as we often see higher baseline pressures.
Dominique Jacobs
September 16, 2025 AT 19:02Listen up, folks-if you’re not checking the max mg/kg before you jab, you’re just asking for trouble! Grab the dosage calculator, plug in the weight, and respect the ceiling; no excuses! Fast, steady, and with proper aspiration, you’ll avoid a toxic spike that could send someone to the ER. Stay sharp, keep the vibe chill, but never compromise safety. Push the best practice, and the patients will thank you.
Dawn Mich
September 17, 2025 AT 00:35Don't be fooled by that so‑called 'best practice' hype-big pharma pushes epinephrine doses to keep us dependent!! They hide the true risks behind glossy charts, and the emergency kits are just a placebo for the scared!!! Wake up, question the agenda, and demand real transparency before the next injection!!!
Eric Sevigny
September 17, 2025 AT 06:08Actually, the key is simple-always test aspirate before you inject, and keep an eye on the vitals. Even a tiny slip can cause a systemic uptake, which is why we keep a spare syringe nearby. A quick double‑check of the dosage chart will catch most errors. And yes, using a 27‑g needle does reduce tissue trauma, even if you typo it in the notes.
Glenda Rosa
September 17, 2025 AT 11:42While the checklist reads like a textbook, real-world dentistry thrives on improvisation-yes, you need safety, but you also need the freedom to adapt. The overemphasis on epinephrine limits could stifle innovative anesthesia blends that seasoned clinicians have crafted for decades. Surely, the blanket warnings ignore nuanced patient histories that only a seasoned practitioner can parse. Thus, I champion a balanced approach: respect the limits, yet trust your clinical intuition to navigate the gray zones.
Francisco Garcia
September 17, 2025 AT 17:15Your perspective adds a valuable layer to the discussion, reminding us that strict protocols shouldn't silence seasoned judgment. I agree that flexibility is key, especially when dealing with diverse patient backgrounds and cultural expectations. At the same time, integrating a quick digital check-like the dosage calculator-can serve as a safety net without cramping creativity. Let’s keep sharing these nuanced views to refine our collective practice.
Patrick Renneker
September 17, 2025 AT 22:48It is incumbent upon the practitioner to adhere scrupulously to the established pharmacological thresholds delineated for each amide local anesthetic, for deviation therefrom may precipitate iatrogenic systemic toxicity with potentially fatal sequelae. The pre‑operative assessment must commence with a comprehensive review of comorbid conditions, inclusive of cardiovascular pathology, hepatic insufficiency, and renal impairment, each of which imposes distinct constraints upon the metabolic clearance of lidocaine, articaine, and mepivacaine. Moreover, the practitioner ought to obtain a meticulous medication inventory, encompassing antihypertensives, anticoagulants, and monoamine oxidase inhibitors, as these agents modulate both the hemodynamic response to epinephrine and the hepatic enzymatic pathways responsible for anesthetic catabolism. Following this, the calculation of the maximum permissible dose must be performed utilising the patient’s weight in kilograms, multiplied by the drug‑specific mg/kg ceiling, whilst incorporating a prudent safety margin of twenty percent to mitigate inadvertent overdosing. The selection of a 27‑gauge needle, coupled with a deliberate aspiration manoeuvre prior to deposition, serves to attenuate the risk of intra‑vascular injection, thereby precluding rapid systemic absorption. Subsequent injection should be administered at a controlled rate, not exceeding one milliliter per fifteen seconds, to further diminish peak plasma concentrations. Continuous intra‑operative monitoring, encompassing pulse oximetry and periodic blood pressure measurement, provides early detection of emergent adverse phenomena such as hypoxia, tachycardia, or hypertensive crises. In the event of discernible signs of local anesthetic systemic toxicity-namely circumoral tingling, metallic taste, auditory disturbances, or altered consciousness-the clinician must be prepared to institute immediate resuscitative measures, including airway support and intravenous lipid emulsion therapy. Documentation of the anesthetic agent, concentration, total dose administered, and any intra‑operative complications constitutes an indispensable component of medicolegal compliance. Post‑procedural directives should advise patients to avoid hot consumables while numbness persists, to monitor for persistent paresthesia beyond the expected duration, and to seek prompt medical attention should systemic symptoms emerge. In summation, the judicious integration of thorough pre‑assessment, precise dosage calculation, meticulous technique, vigilant monitoring, and comprehensive patient education coalesces to substantially curtail the incidence of dental local anesthetic complications.
KAYLEE MCDONALD
September 18, 2025 AT 04:22Your thorough protocol reminds us that safety must never be compromised.