Cardiac Inflammation: Causes, Symptoms, and Treatment Options
When working with cardiac inflammation, the swelling of heart tissue caused by infection, auto‑immune response, toxins, or medication side effects. Also known as myocarditis, it can affect the heart muscle itself or the surrounding sac, reducing the organ’s ability to pump blood efficiently. Common triggers include viral infections like Coxsackie or COVID‑19, bacterial infections such as Lyme disease, autoimmune disorders (e.g., lupus), and certain chemotherapy agents. Early signs often feel like unexplained fatigue, shortness of breath, chest discomfort, or irregular heartbeats, and they signal that the heart’s electrical system may be under stress. Because the heart has limited capacity to heal on its own, recognizing these warnings early can prevent permanent damage and improve long‑term outcomes.
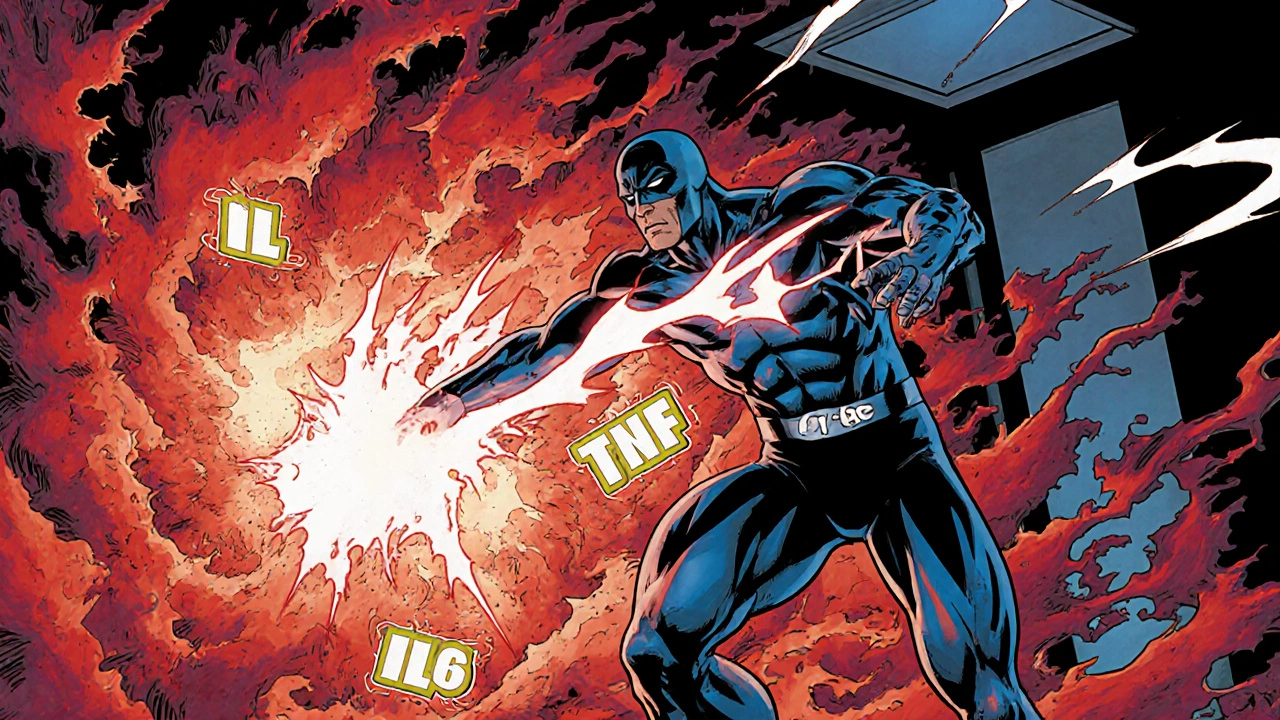
One major subtype is myocarditis, inflammation of the heart muscle that typically follows viral exposure and can progress to heart failure if untreated. Another is pericarditis, inflammation of the pericardial sac, often presenting as sharp chest pain that worsens when lying flat. A less common but serious form is endocarditis, infection of the inner heart lining, usually linked to bacterial entry via bloodstream. Managing cardiac inflammation frequently requires anti‑inflammatory medication. First‑line agents are NSAIDs, non‑steroidal anti‑inflammatory drugs such as ibuprofen that relieve pain and reduce swelling. When inflammation is severe or persistent, clinicians may add corticosteroids, potent steroids like prednisone that suppress the immune response and limit tissue damage. In specific autoimmune cases, disease‑modifying agents or biologics might be introduced to target the underlying immune dysregulation.
Accurate diagnosis hinges on a combination of laboratory and imaging tools. Elevated cardiac biomarkers, particularly troponin, signal muscle injury, while an electrocardiogram can reveal arrhythmias or ST‑segment changes typical of inflammation. Echocardiography provides a real‑time view of heart function, showing reduced ejection fraction or pericardial effusion when present. Cardiac MRI offers detailed tissue characterization, confirming edema and fibrosis that define myocarditis. These diagnostic imaging techniques help clinicians assess cardiac inflammation and guide therapy intensity. Lifestyle advice also plays a role: patients are encouraged to avoid strenuous exercise until inflammation resolves, maintain a heart‑healthy diet, and manage stress. Follow‑up appointments monitor recovery, and repeat imaging ensures that scar formation does not compromise future cardiac performance. Below you’ll find a curated set of articles that dive deeper into drug interactions, specific treatment comparisons, and practical management tips related to cardiac inflammation and its many faces.