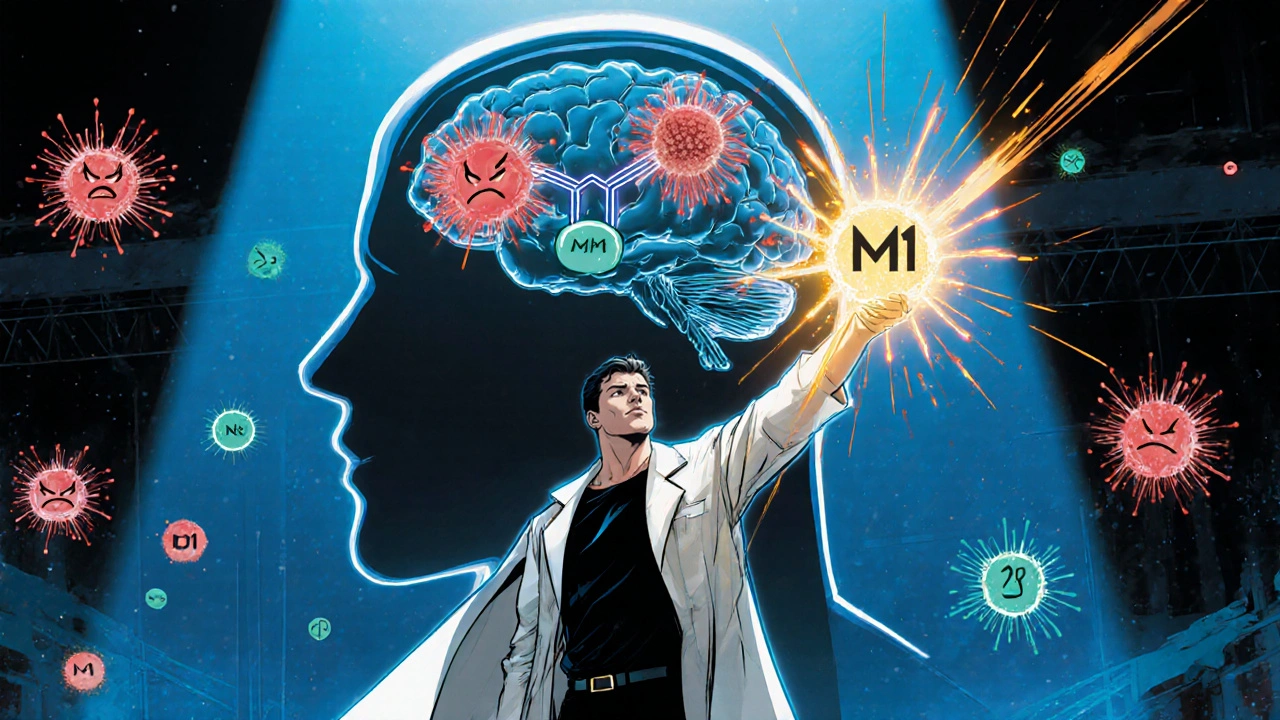
Neuroinflammation
When dealing with Neuroinflammation, the brain’s inflammatory response that can drive or worsen neurological conditions. Also known as brain inflammation, it involves immune cells, signaling molecules, and vascular changes.
One of the main culprits behind this response is Microglia, the resident immune cells of the central nervous system. When they sense danger—whether from infection, trauma, or misfolded proteins—they shift from a resting to an activated state. This shift is a core part of the semantic triple: Neuroinflammation encompasses microglial activation. Activated microglia release a flood of Cytokines, signaling proteins that coordinate the inflammatory cascade, such as IL-1β, TNF‑α, and IL‑6.
Key players in neuroinflammation
Those cytokines don’t act in isolation. They can compromise the Blood‑Brain Barrier, the selective filter that protects the brain from circulating toxins and pathogens. When the barrier leaks, peripheral immune cells slip in, adding fuel to the fire. This creates the second semantic link: Neuroinflammation influences cytokine release. The third link follows naturally: Blood‑brain barrier disruption exacerbates neuroinflammation. Understanding how these three entities interact helps you see why a single trigger can spiral into chronic brain inflammation.
Why does this matter for everyday health? Research shows that prolonged neuroinflammation is a common thread in Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and even mood disorders. The brain’s immune environment can tip the scales from normal aging to neurodegeneration. For someone managing a chronic condition, recognizing the signs—persistent headaches, cognitive fog, mood swings—can prompt early intervention.
Speaking of intervention, lifestyle choices play a surprisingly big role. Diets rich in omega‑3 fatty acids, antioxidants, and low‑glycemic foods have been shown to dampen microglial activation. Regular aerobic exercise boosts circulation, helping the blood‑brain barrier stay tight and reducing systemic inflammation that would otherwise seep into the brain.
Pharmacologic options target the same pathways. Certain antiviral or anti‑inflammatory drugs listed in our collection—like acyclovir or cefuroxime—can indirectly affect neuroinflammatory processes by clearing infections that would otherwise spark an immune response. Meanwhile, steroids, NSAIDs, and newer agents such as cytokine inhibitors directly blunt the signaling cascade.
It’s also worth noting that not every inflammation is bad. Short‑term, well‑controlled neuroinflammation is essential for debris clearance after injury and for neuroplasticity. The goal isn’t to eliminate inflammation entirely, but to keep it balanced. That’s why monitoring biomarkers—like C‑reactive protein or specific cytokine panels—can guide treatment intensity.
For clinicians and patients alike, the challenge is spotting the point where normal healing becomes harmful. Our articles on drug interactions, side‑effect profiles, and disease‑specific guidelines give concrete steps to navigate that line. For example, the piece on acyclovir interactions warns about kidney strain, a concern because impaired renal function can amplify systemic inflammation and worsen neuroinflammatory outcomes.
Another practical angle is the role of hormone therapy, especially during menopause. Hormonal shifts can alter cytokine production and affect the blood‑brain barrier’s integrity. The menopause‑related vertigo article highlights how balance exercises can support vestibular function, indirectly reducing stress‑related inflammatory spikes.
Technology also enters the picture. Wearable devices that track sleep, heart rate variability, and inflammatory markers empower patients to catch early signs of neuroinflammatory flare‑ups. Telemedicine visits make it easier to adjust medication doses—like verapamil or abacavir—based on real‑time data.
Putting all this together, you now have a roadmap: identify triggers, support the barrier, modulate microglial activity, and use targeted therapies when needed. The posts below dive deeper into each of these steps, offering drug‑specific guidance, lifestyle tweaks, and patient stories that illustrate how to apply this knowledge in real life.
Ready to explore the details? Scroll down to find evidence‑based articles that break down interactions, dosing, and practical tips for managing neuroinflammation across a range of conditions.