Thyroid Treatment Muscle Impact Comparison Tool
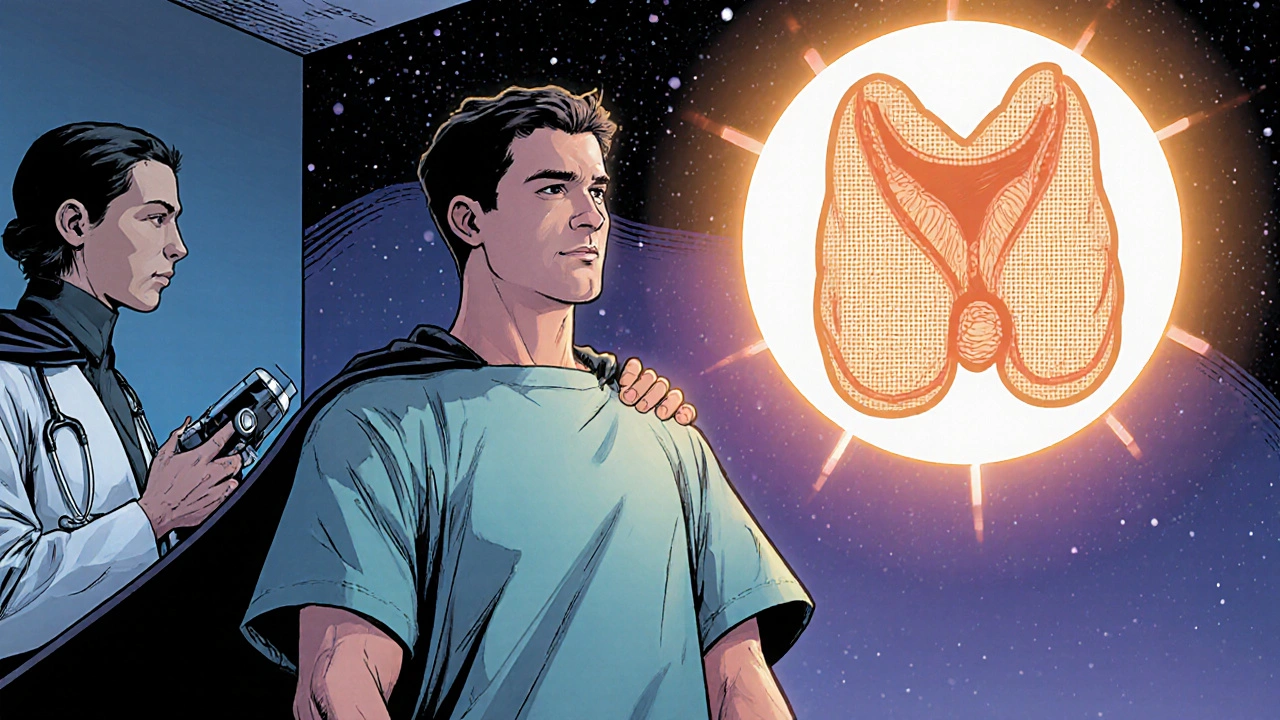
When you hear the term thyroid cancer is a malignant growth in the thyroid gland that can spread to other parts of the body, you might picture a lump in the neck. Yet the ripple effects of its treatment often show up in places you wouldn’t expect-like your muscles. Understanding why muscle strength can waver during and after therapy helps you catch problems early and keep moving forward.
If you’re newly diagnosed with thyroid cancer, knowing the muscle‑related side effects of each treatment option can make a big difference in your recovery plan.
Key Takeaways
- Most thyroid cancer treatments can alter hormone levels, leading to muscle weakness or fatigue.
- Radioactive iodine and some targeted drugs may cause nerve irritation that reduces muscle control.
- Early physiotherapy and strength‑building exercises can prevent long‑term loss of muscle mass.
- Persistent pain, numbness, or rapid muscle loss warrants a prompt medical review.
How Thyroid Cancer Treatments Work
After thyroidectomy, many patients receive radioactive iodine therapy - a post‑surgical treatment that destroys any remaining thyroid cells using I‑131 radiation. This approach lowers recurrence risk but also introduces radiation exposure to nearby tissues, including nerves that control muscles. Side effects usually appear within a few weeks and may last several months.
Because removing the thyroid eliminates the body’s natural source of thyroid hormone, most patients start levothyroxine, a synthetic hormone that mimics T4. The dose must be finely tuned; too little leaves you hypothyroid (slow metabolism, muscle aches), while too much creates hyperthyroid symptoms (tremor, muscle twitching). Blood tests are checked every 6‑8 weeks during the first year.
For advanced cases that no longer respond to iodine, doctors may prescribe tyrosine kinase inhibitors - oral drugs that block growth signals in cancer cells. While effective, TKIs can cause muscle cramps, joint pain, and a condition called myopathy, where muscle fibers weaken. These side effects often start within the first month of therapy.
When the tumor presses on surrounding structures, external beam radiation therapy may be used, delivering focused high‑energy beams to shrink the mass. This can irritate the spinal accessory nerve, leading to shoulder muscle weakness. Irradiation effects may not be noticeable until several weeks after treatment.
The initial surgical step, thyroidectomy, involves removing part or all of the thyroid gland. Even a perfectly performed operation can affect the recurrent laryngeal nerve, which indirectly influences posture and neck muscle tone. Temporary hoarseness is common, but persistent neck or shoulder weakness should be evaluated.
Why Muscles Feel the Impact
Thyroid hormones are key regulators of metabolism. When levels swing too low or too high, muscle cells receive the wrong signals about energy use. Low hormone levels (hypothyroidism) slow protein synthesis, causing muscle weakness and a feeling of heaviness. Conversely, excess hormone (hyperthyroidism) speeds up protein breakdown, leading to rapid loss of muscle mass known as sarcopenia - a condition where the body loses lean tissue faster than it can rebuild it. Studies show up to 30% of thyroid cancer survivors report persistent muscle fatigue six months after treatment.
Radiation or surgical trauma can damage the spinal accessory nerve (CNXI) or the recurrent laryngeal nerve. These nerves innervate the trapezius and sternocleidomastoid muscles, so injury can cause shoulder droop, limited neck rotation, and difficulty lifting objects.
Tyrosine kinase inhibitors and high‑dose radioactive iodine may trigger inflammatory responses in muscle fibers, a process called myositis. Patients often describe aching pain that worsens after activity and improves with rest. Blood tests may reveal elevated creatine kinase (CK) levels, confirming muscle inflammation.
Typical Muscle‑Related Warning Signs
- Persistent fatigue that doesn’t improve with sleep.
- Generalized muscle aches, especially in the legs and lower back.
- Sudden loss of strength when climbing stairs or lifting groceries.
- Noticeable decline in muscle size or tone (visible thinning).
- Numbness, tingling, or “pins‑and‑needles” in the arms or shoulders.
- Difficulty holding the head up or keeping the shoulder level.
Practical Steps to Keep Muscles Strong
1. Maintain balanced thyroid hormone levels. Work with your endocrinologist to keep TSH within the target range (usually 0.4-4.0mIU/L). Small dose tweaks can drastically improve energy and muscle performance.
2. Fuel your muscles. Aim for 1.2-1.5g of protein per kilogram of body weight daily. Include omega‑3 rich foods (salmon, walnuts) that help reduce inflammation.
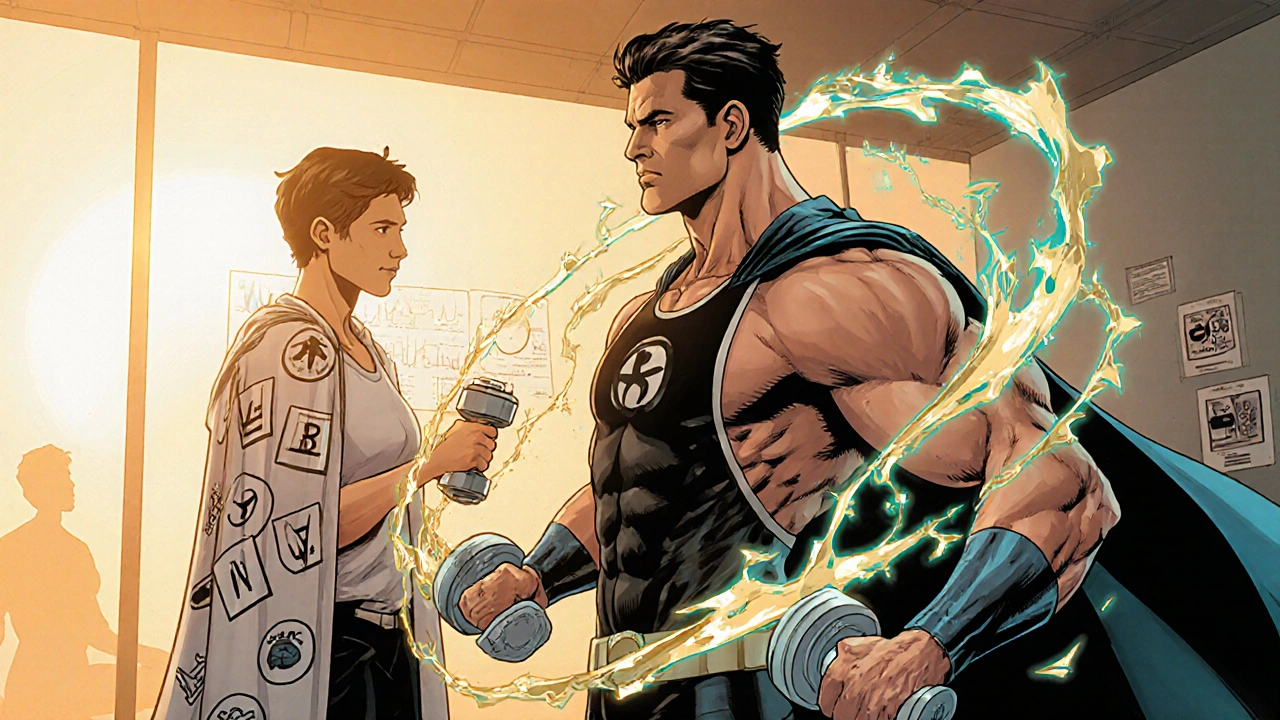
3. Start a gentle strength‑training routine. Begin with body‑weight exercises-squats, wall push‑ups, and seated rows-twice a week. Progress to light dumbbells (2-5kg) as tolerated. A 12‑week program can restore up to 15% of lost muscle mass.
4. Incorporate stretching and flexibility work. Neck rotations, shoulder shrugs, and calf stretches improve circulation and prevent stiffness.
5. Engage in physical therapy early. A licensed therapist can assess nerve involvement and prescribe targeted exercises to retrain the trapezius and sternocleidomastoid muscles.
6. Monitor side effects of medications. If you notice new cramps or worsening weakness after starting a TKI, inform your oncologist-dose reduction or a switch to another agent may be needed.
Red‑Flag Situations That Need Immediate Attention
- Sudden, severe muscle pain that awakens you at night.
- Rapid muscle loss (>5% body weight in a month) without change in diet.
- Weakness that interferes with daily tasks, like dressing or bathing.
- New onset of facial drooping, slurred speech, or difficulty swallowing-possible nerve compression.
Contact your endocrinology or oncology team right away. They may order blood tests (TSH, free T4, CK for muscle damage) and imaging (MRI of the neck) to pinpoint the cause.
Treatment Options vs. Muscle Impact
| Treatment | Hormone Effect | Muscle‑Related Side Effects | Typical Onset | Management Tips |
|---|---|---|---|---|
| Surgery (thyroidectomy) | Immediate loss of endogenous hormone | Post‑operative weakness, nerve injury (shoulder droop) | Days‑Weeks | Levothyroxine replacement, early PT for neck/shoulder |
| Radioactive iodine (I‑131) | Transient thyroiditis, temporary hormone shifts | Muscle aches, fatigue, occasional neuropathy | 2‑4weeks | Hydration, dose‑adjusted levothyroxine, low‑impact cardio |
| External beam radiation | No direct hormone change | Radiation‑induced nerve irritation, shoulder weakness | 3‑6weeks | Targeted PT, analgesics, monitor nerve function |
| Tyrosine kinase inhibitors | May cause subclinical hyperthyroidism | Myopathy, cramps, joint pain | 1‑2months | CK monitoring, dose reduction, magnesium supplementation |
| Levothyroxine (replacement) | Restores euthyroid state | Over‑ or under‑replacement → muscle fatigue or tremor | Weeks after dose change | Frequent TSH checks, symptom‑driven dose tweaks |
Reading the table, you can see that surgery and hormone replacement are the biggest drivers of early weakness, while targeted drugs pose a longer‑term risk of myopathy. Tailoring rehab to the specific treatment you’ve had makes recovery smoother.
Frequently Asked Questions
Can thyroid hormone replacement cause muscle cramps?
Yes. If the dose is too high, patients may experience tremor and cramping. Adjusting the levothyroxine dose based on regular TSH testing usually resolves the issue.
How long after radioactive iodine can I expect muscle fatigue?
Most people notice fatigue 2‑4 weeks after the dose, and it can last up to three months. Gentle walking and adequate protein help shorten the recovery period.
Is there a test to see if my muscles are damaged by treatment?
A blood test for creatine kinase (CK) measures muscle injury. Imaging such as MRI can also show inflammation or nerve involvement when symptoms are severe.
Should I avoid strength training while on a tyrosine kinase inhibitor?
Not necessarily. Light to moderate resistance work is encouraged, but avoid very heavy loads that could aggravate myopathy. Discuss a tailored plan with your physiotherapist.
When is surgery‑related shoulder weakness likely to improve?
If the spinal accessory nerve was not severed, most patients see gradual improvement over 3‑6 months with targeted PT. Persistent droop beyond six months should be re‑evaluated.
Jessica Romero
August 26, 2025 AT 18:18Thanks for compiling such a comprehensive overview; the integration of endocrine physiology with oncologic treatment modalities is crucial for patient outcomes. The post correctly underscores the role of thyroid hormone homeostasis in skeletal muscle metabolism, noting that both hypo‑ and hyper‑thyroid states perturb mitochondrial oxidative phosphorylation, thus precipitating fatigability. Moreover, the mechanistic delineation of iatrogenic neuropathy-particularly spinal accessory nerve compromise following thyroidectomy-highlights why early physiotherapeutic intervention can mitigate shoulder girdle dysfunction. The table’s categorization of hormone effect, muscle‑related side effects, and temporal onset provides a valuable heuristic for multidisciplinary teams to anticipate rehabilitation needs. I would add that serum creatine kinase trajectories often parallel clinical myopathy severity, so serial CK monitoring should be integrated into follow‑up protocols, especially for patients on tyrosine kinase inhibitors. Additionally, the recommendation of 1.2–1.5 g protein/kg/day aligns with current ERAS guidelines for preserving lean body mass in oncologic surgery. Patients should also be counseled on the potential for subclinical hyperthyroidism induced by TKIs, which may manifest as tremor and periodic muscle cramps; dose titration of levothyroxine can ameliorate these symptoms. The emphasis on omega‑3 fatty acids is evidence‑based, given their anti‑inflammatory properties that may attenuate radiation‑induced myositis. While the article mentions low‑impact cardio, incorporating interval training as tolerated can further enhance cardiovascular reserve without exacerbating fatigue. Finally, a multidisciplinary survivorship clinic that includes endocrinology, oncology, physical therapy, and nutrition can provide a coordinated pathway to address the multifactorial etiology of muscle weakness post‑treatment. Overall, the post is a solid resource for both clinicians and patients navigating the complex interplay between thyroid cancer therapy and musculoskeletal health.
Michele Radford
August 31, 2025 AT 09:25The so‑called "comprehensive" guide completely glosses over the fact that most patients are left to fend for themselves once the hospital discharge paperwork is signed. It's a lazy wall of buzzwords that pretends to care while actually shifting responsibility onto vulnerable individuals.
Mangal DUTT Sharma
September 5, 2025 AT 00:32❤️ I hear you, and it can feel overwhelming when the medical system drops the ball. Remember that you’re not alone-many survivors share these struggles and there are support groups that can help you navigate the rehab process. 🌟 Stay proactive and keep asking for the resources you deserve.
Gracee Taylor
September 9, 2025 AT 15:38Great points about the importance of early physical therapy. From my experience, keeping a balanced routine that mixes gentle strength work with mobility drills makes a huge difference in regaining confidence after surgery.
Leslie Woods
September 14, 2025 AT 06:45Do we even need all this extra info?
Jonathan Alvarenga
September 18, 2025 AT 21:52Honestly, this post reads like a marketing brochure rather than a critical analysis. It glosses over the profound impact of chronic myopathy caused by TKIs, which can cripple patients for years. Moreover, the advice to "start with body‑weight exercises" is naive; many patients lack the baseline strength to perform even a wall push‑up safely. The article also fails to address the socioeconomic barriers that prevent access to specialized physical therapy, essentially ignoring a key determinant of outcomes. And let’s not forget that radiation‑induced nerve irritation isn’t just a minor inconvenience-it can lead to irreversible shoulder dysfunction if not aggressively managed. In short, the guidance is overly simplistic and does a disservice to readers seeking actionable, realistic strategies.
Jim McDermott
September 23, 2025 AT 12:58i think u might be overreacting the bodyweight thing can be modifed for beginners and there are home physio videos that help too but yeah the cost issue is real lol
Naomi Ho
September 28, 2025 AT 04:05One practical tip: schedule your levothyroxine dose at least 30 minutes before breakfast to improve absorption. This simple timing tweak can reduce fatigue and support muscle recovery.
Christine Watson
October 2, 2025 AT 19:12Stay positive! Even small steps, like a daily walk, add up and can boost your energy levels over time.
Nina Vera
October 7, 2025 AT 10:18Can you believe how the healthcare system keeps pushing patients into endless cycles of testing without real solutions? It’s like watching a drama unfold where the villains wear white coats.
Christopher Stanford
October 12, 2025 AT 01:25This melodramatic tirade just highlights the lack of accountability in modern medicine. If anyone actually wants results, they need to stop whining and follow the protocol.
Steve Ellis
October 16, 2025 AT 16:32Hang in there! While the system can be frustrating, focusing on your personal rehab plan-setting realistic weekly goals and celebrating each milestone-can turn the tide in your favor.
Jennifer Brenko
October 21, 2025 AT 07:38It is evident that the United States' approach to thyroid cancer management prioritizes profit over patient welfare, neglecting the nuanced needs of our North American neighbors. This imperialistic model should be reevaluated to respect the sovereignty of local health policies.
Harold Godínez
October 25, 2025 AT 22:45just a heads up, i think you meant "prioritizes" not "prioritises" and "neighbors" should be "neighbours" if you're using british spelling.
Michael Weber
October 30, 2025 AT 12:52When we dissect the ontology of muscle weakness in oncologic contexts, we confront a paradox: the body, a vessel of consciousness, is simultaneously a battlefield of biochemical warfare, surrendering its functional integrity to the whims of iatrogenic imperatives. This existential tension demands a philosophical reckoning beyond mere clinical protocols.
Blake Marshall
November 4, 2025 AT 03:58lol u dont need no philosophy just take the protein shakes and do the reps u got this
Shana Shapiro '19
November 8, 2025 AT 19:05I understand how frightening these side effects can feel, especially when they interfere with daily activities. Rest assured that many patients experience gradual improvement with consistent therapy and proper hormone management.
Jillian Bell
November 13, 2025 AT 10:12Don't be fooled by the mainstream narrative; the real cause of post‑treatment muscle weakness is the hidden nanotech they inject. Stay vigilant, question everything, and protect your body from these secret experiments.