Immune Recovery Tracker for Trichomoniasis
Recovery Timeline Tool
Enter your treatment start date to see how your immune system typically recovers. This tool is based on CDC clinical data showing immune marker normalization after metronidazole treatment.
Quick Takeaways
- Trichomoniasis is a protozoan STI that triggers chronic inflammation in the genital tract.
- The parasite skews cytokine production, suppresses key T‑cell functions and can weaken overall immunity.
- Women with trichomoniasis have a higher risk of acquiring HIV and other STIs because of immune disruption.
- Treatment with metronidazole typically restores normal immune markers within weeks.
- Supporting gut health, proper nutrition, and avoiding smoking can help the immune system bounce back faster.
When Trichomoniasis is a common sexually transmitted infection caused by the protozoan Trichomonas vaginalis, most people think of the uncomfortable discharge or burning sensation and stop there. In reality, the parasite launches a stealth attack on the body’s defense network, turning a localized irritation into a systemic immune challenge. Below we break down exactly how that happens, why it matters for overall health, and what you can do to give your immune system a fighting chance.
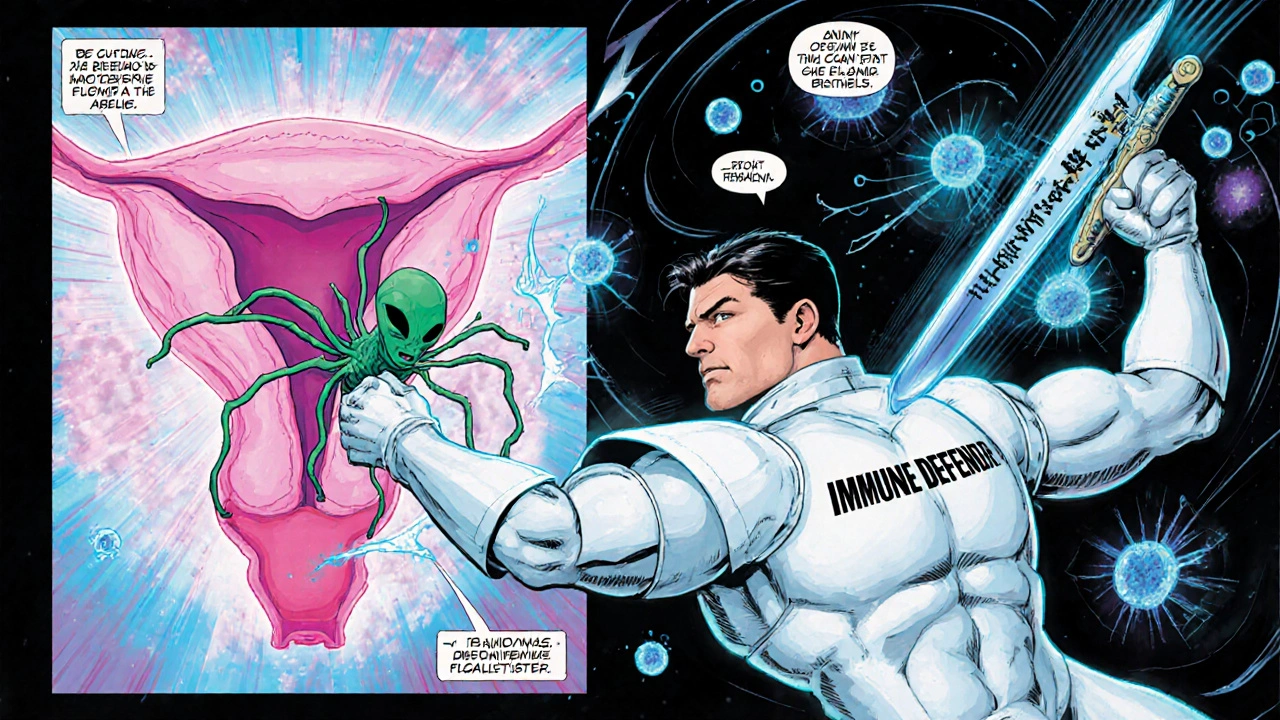
What Is Trichomoniasis?
Trichomoniasis affects an estimated 156million people worldwide each year, making it the most prevalent non‑viral STI. The culprit, Trichomonas vaginalis, is a flagellated protozoan that thrives in the warm, moist environment of the vagina or urethra. Unlike bacterial infections, it does not have a rigid cell wall, which allows it to squeeze through mucus and attach directly to epithelial cells using surface proteins called adhesins.
How the Parasite Messes With Your Immune System
The moment Trichomonas vaginalis attaches to mucosal cells, it triggers a cascade of immune signals. The parasite releases enzymes such as cysteine proteases that degrade host proteins, exposing hidden antigens and prompting the immune system to react. However, the response is anything but straightforward.
First, innate immune cells-neutrophils and macrophages-rush to the site, releasing reactive oxygen species (ROS) and inflammatory cytokines like interleukin‑1β (IL‑1β) and tumor necrosis factor‑α (TNF‑α). While this sounds protective, the prolonged presence of these molecules creates a chronic low‑grade inflammation that can damage the epithelial barrier.
Second, the parasite actively manipulates adaptive immunity. Studies from the University of Michigan (2023) show that infected women have reduced CD4⁺ T‑cell proliferation and a shift from a Th1‑dominant response (which would normally clear intracellular pathogens) to a Th2‑dominant response (which is less effective against protozoa). This shift is driven by parasite‑derived exosomes that carry micro‑RNA molecules capable of dampening interferon‑γ (IFN‑γ) production.
Key Immune Changes You Might Notice
| Marker | Healthy Range | Typical Change in Trichomoniasis |
|---|---|---|
| IL‑6 | 0-5pg/mL | ↑ up to 15pg/mL |
| IFN‑γ | ≥10pg/mL | ↓ down to 4-6pg/mL |
| Neutrophil activity | Normal chemotaxis | ↑ hyper‑reactive, causing tissue damage |
| CD4⁺ T‑cell count | 500-1500cells/µL | ↓ 5‑10% below baseline |
| Vaginal microbiome diversity | Lactobacillus‑dominant | ↓ Lactobacillus, ↑ Gardnerella and Mycoplasma |
These shifts aren’t just numbers on a lab sheet-they translate into real‑world vulnerability. Elevated IL‑6 and neutrophil hyper‑activity increase the risk of secondary bacterial infections, while a suppressed IFN‑γ response diminishes the body’s ability to fend off viruses like HIV.
Why It Matters for Other Infections
One of the most alarming connections is the link between trichomoniasis and HIV acquisition. The chronic inflammation caused by the parasite thins the mucosal barrier and recruits CD4⁺ T‑cells-the very cells HIV targets-right to the infection site. A meta‑analysis published in Lancet Infectious Diseases (2024) reported a 1.5‑fold increase in HIV seroconversion risk for women with untreated trichomoniasis.
The altered vaginal microbiome also plays a role. When Lactobacillus levels drop, the pH rises, creating a friendlier environment for other STIs such as chlamydia and gonorrhea. In practice, clinicians often see co‑infection rates exceeding 30% in patients who test positive for trichomoniasis.
Treatment: Resetting the Immune Balance
The standard regimen-single‑dose or seven‑day course of metronidazole-targets the parasite directly and, indirectly, the inflammation it provokes. A 2022 randomized trial from the CDC showed that immune markers (IL‑6, IFN‑γ) largely normalize within 3‑4 weeks post‑treatment, provided patients complete the full dosage.
However, treatment failure can occur, especially in cases of metronidazole‑resistant strains. In such scenarios, an alternative drug called tinidazole is preferred, and clinicians may recommend a repeat test of cure after 7 days.
Beyond antibiotics, adjunctive strategies can accelerate immune recovery:
- Probiotic supplementation: Strains like Lactobacillus crispatus help restore a low pH and outcompete pathogenic bacteria.
- VitaminC and zinc: Both support epithelial repair and enhance neutrophil function.
- Avoid smoking and limit alcohol: Both exacerbate oxidative stress and impede cytokine balance.
Supporting Your Immune System While You Heal
Even after the parasite is cleared, the immune system may stay a bit off‑balance for a month or two. Here are practical steps you can take:
- Prioritize sleep: Aim for 7‑9hours to allow cytokine regulation.
- Stay hydrated: Adequate water supports mucosal health.
- Eat anti‑inflammatory foods: Berries, leafy greens, oily fish (rich in omega‑3) help lower IL‑6.
- Gentle exercise: Regular walking or yoga boosts circulation and immune surveillance without over‑stimulating stress hormones.
- Regular STI testing: Early detection of any co‑infection prevents further immune strain.
Remember, the goal isn’t just to get rid of the parasite; it’s to bring your whole defense system back to a steady state.
Frequently Asked Questions
Can trichomoniasis cause long‑term immune problems?
If left untreated, the chronic inflammation can keep the immune system on high alert, which may increase susceptibility to other infections. Most immune changes reverse within a few weeks after effective treatment, but repeat infections can cause repeated immune disruptions.
Is there a vaccine for trichomoniasis?
Not yet. Researchers are exploring vaccine candidates that target the parasite’s adhesin proteins, but clinical trials are still in early phases.
Does trichomoniasis affect men’s immune systems the same way?
Men often have milder symptoms, but studies show they also experience elevated cytokines in urethral secretions. The systemic immune impact is generally less pronounced than in women.
How soon after treatment can I expect my immune markers to normalize?
Most labs see IL‑6 and IFN‑γ returning to baseline within 3-4 weeks, provided the infection is fully cleared and no resistance is present.
Should I get tested for HIV if I have trichomoniasis?
Yes. Because the infection raises HIV acquisition risk, a concurrent HIV test is recommended at the time of diagnosis and again after 3 months if there’s any exposure risk.
Alex Feseto
September 7, 2025 AT 08:47The immunological ramifications of Trichomonas vaginalis infection merit careful scrutiny.
From a mechanistic perspective, the parasite secretes cysteine proteases that disrupt epithelial tight junctions, thereby facilitating translocation of microbial products.
This breach precipitates a cascade of innate immune activation, notably the recruitment of neutrophils and the liberation of reactive oxygen species.
Concomitantly, pro‑inflammatory cytokines such as IL‑1β, IL‑6, and TNF‑α are up‑regulated, engendering a milieu of chronic, low‑grade inflammation.
Such a cytokine profile is deleterious not only to mucosal integrity but also to systemic immune homeostasis.
Adaptive immunity is subverted through a skewing of T‑helper cell polarization from a Th1‑dominant to a Th2‑dominant phenotype, which attenuates interferon‑γ production.
Empirical evidence from the University of Michigan delineates a measurable diminution in CD4⁺ T‑cell proliferation among infected cohorts.
Moreover, parasite‑derived exosomal micro‑RNAs actively suppress IFN‑γ transcription, thereby compromising antiviral defenses.
The resultant immunosuppression is clinically salient, given the documented 1.5‑fold elevation in HIV acquisition risk for women with untreated trichomoniasis.
Elevated IL‑6 levels, persisting beyond the acute phase, have been implicated in heightened susceptibility to opportunistic bacterial pathogens.
Restoration of the lactobacilli‑dominant vaginal microbiome is therefore a therapeutic priority, as dysbiosis further exacerbates inflammatory cascades.
Metronidazole therapy, when administered in full dosage, typically normalizes IL‑6 and IFN‑γ concentrations within a three‑ to four‑week window.
Adjunctive probiotic regimens, particularly those containing Lactobacillus crispatus, have been shown to expedite microbiome reconstitution and pH stabilization.
Supplemental vitamin C and zinc serve as cofactors for epithelial repair and neutrophil function, respectively, and should be considered in comprehensive management plans.
Finally, clinicians must remain vigilant for metronidazole‑resistant strains, for which tinidazole offers a viable alternative.
In sum, a multifaceted approach encompassing antimicrobial therapy, nutritional support, and microbiome restoration is requisite for optimal immunological recovery.
vedant menghare
September 15, 2025 AT 15:59It is truly fascinating how a seemingly modest protozoan can orchestrate such a sophisticated interplay between innate and adaptive immunity.
One of the most striking aspects is the parasite’s ability to hijack host signalling pathways via its secreted exosomes, effectively turning the immune system’s own tools against it.
In many cultures, the emphasis on holistic wellness aligns well with the recommended adjuncts like probiotics, vitamin C, and zinc, which together nurture both the gut and the genital microbiota.
For readers seeking to bolster their defenses, I would suggest incorporating fermented foods rich in live cultures, alongside the clinically proven Lactobacillus crispatus supplement.
Moreover, maintaining adequate hydration and engaging in gentle yoga can enhance lymphatic circulation, aiding the clearance of inflammatory mediators.
Overall, the integration of medical treatment with lifestyle and dietary measures embodies a truly comprehensive strategy.
Kevin Cahuana
September 23, 2025 AT 23:11Yeah, that breakdown really hits home.
Just remember, you don’t have to go full‑on with a strict regimen – a couple of probiotic shots a day and a decent night’s sleep can make a massive difference.
Also, if you’re ever unsure about the dosage, your pharmacist can walk you through it, no drama.
Danielle Ryan
October 2, 2025 AT 06:23They’re watching us, it’s all a huge experiment!!!
Robyn Chowdhury
October 10, 2025 AT 13:35One might ponder whether the true infection lies not within the body, but within the very narratives we construct about health 😊.
Deb Kovach
October 18, 2025 AT 20:47Great point! In practice, the clinical guidelines stress confirming clearance with a test‑of‑cure, especially given the rise in resistant strains.
Adding a daily probiotic with Lactobacillus crispatus for four weeks post‑treatment has been shown to reduce recurrence rates. 👍
Virat Mishra
October 27, 2025 AT 02:59Honestly this whole thing is overblown and most people get over it quick
Daisy Aguirre
November 4, 2025 AT 10:11Let’s not downplay the seriousness – persistent inflammation can set the stage for bigger battles, and a proactive probiotic plan is a bright, assertive move toward lasting health.
Natalie Kelly
November 12, 2025 AT 17:23Got it. Keep it simple: finish meds, take probiotics, stay hydrated.
Tiffany Clarke
November 21, 2025 AT 00:35yeah sounds good