HIV Risk Calculator
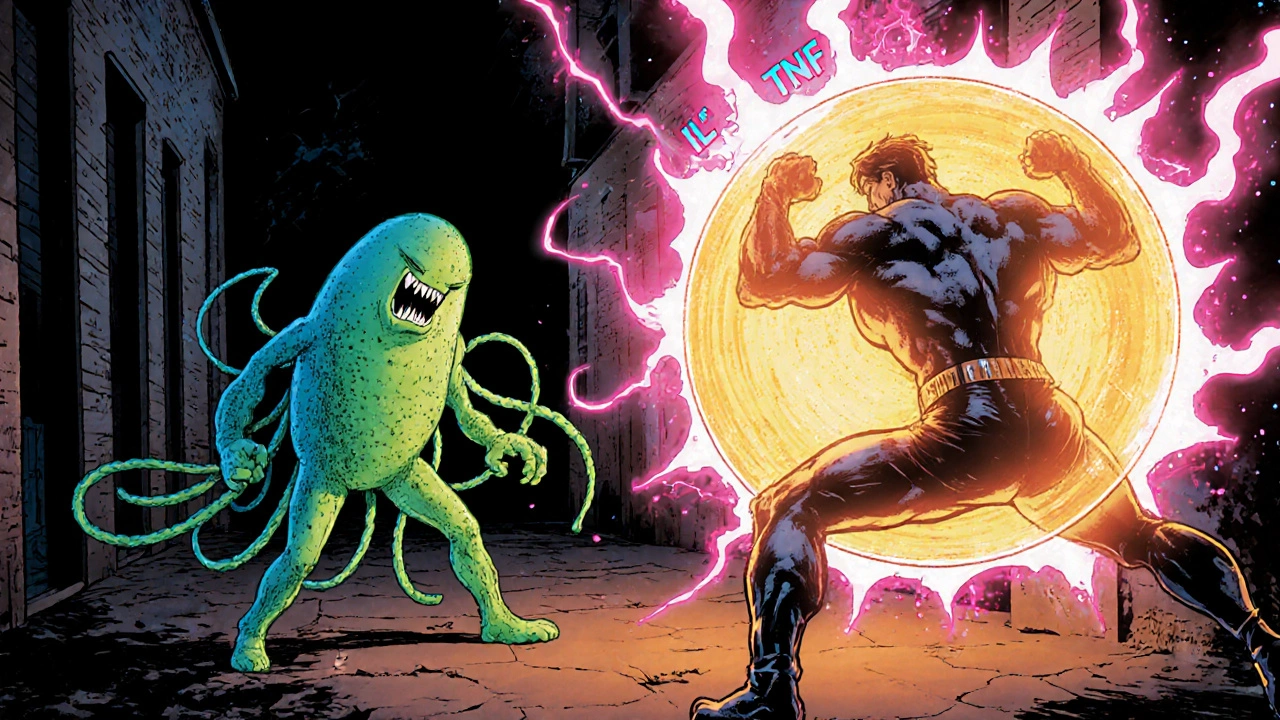
How Trichomoniasis Affects HIV Risk
This tool calculates your relative HIV risk based on whether you have trichomoniasis. Studies show untreated trichomoniasis increases HIV susceptibility by 2.8-fold due to mucosal damage and immune activation.
Ever wondered why a seemingly simple vaginal infection can mess with the rest of your body? That’s because trichomoniasis is more than a local irritation - it talks to your immune system, shifts the balance of tiny microbes in the vagina, and can even raise the odds of catching other infections. Below we break down exactly how this protozoan parasite pulls the strings of your immune defenses and what you can do to keep things in check.
Quick Takeaways
- Trichomoniasis is caused by the protozoan Trichomonas vaginalis, a flagellated parasite that thrives in the low‑oxygen environment of the genital tract.
- The infection triggers a burst of cytokines such as IL‑1β and TNF‑α, creating short‑term inflammation.
- Persistent infection reshapes the vaginal microbiome, lowering protective lactobacilli and inviting opportunistic bacteria.
- Altered immunity can increase susceptibility to HIV by up to three‑fold, largely through mucosal barrier disruption and immune cell recruitment.
- Effective treatment (metronidazole or tinidazole) combined with probiotic support restores balance and reduces lingering immune activation.
Now let’s dig into the science behind each of those points.
What Exactly Is Trichomoniasis?
Trichomoniasis is a sexually transmitted infection (STI) caused by Trichomonas vaginalis, a single‑celled protozoan that measures about 10‑12µm in length. Unlike bacterial STIs, this parasite lives without a cell wall, making it resistant to many antibiotics but vulnerable to nitro‑imidazole drugs. Roughly 156million people worldwide are infected each year, and a large portion never show symptoms, especially men. When symptoms appear, they usually involve itching, discharge, and a burning sensation during urination.
How the Body Detects the Parasite
The moment Trichomonas vaginalis attaches to the epithelial cells of the vagina or urethra, pattern‑recognition receptors (PRRs) on immune cells recognize its surface proteins and flagella. This triggers the innate immune immune system to release a cascade of signaling molecules.
Key players include:
- Cytokines like interleukin‑1β (IL‑1β), interleukin‑6 (IL‑6), and tumor necrosis factor‑alpha (TNF‑α).
- Chemokines such as IL‑8 that attract neutrophils to the infection site.
- Antimicrobial peptides (AMPs) - small proteins that directly attack microbes, e.g., defensins and cathelicidins.
These molecules create a rapid inflammatory response aimed at flushing out the parasite.
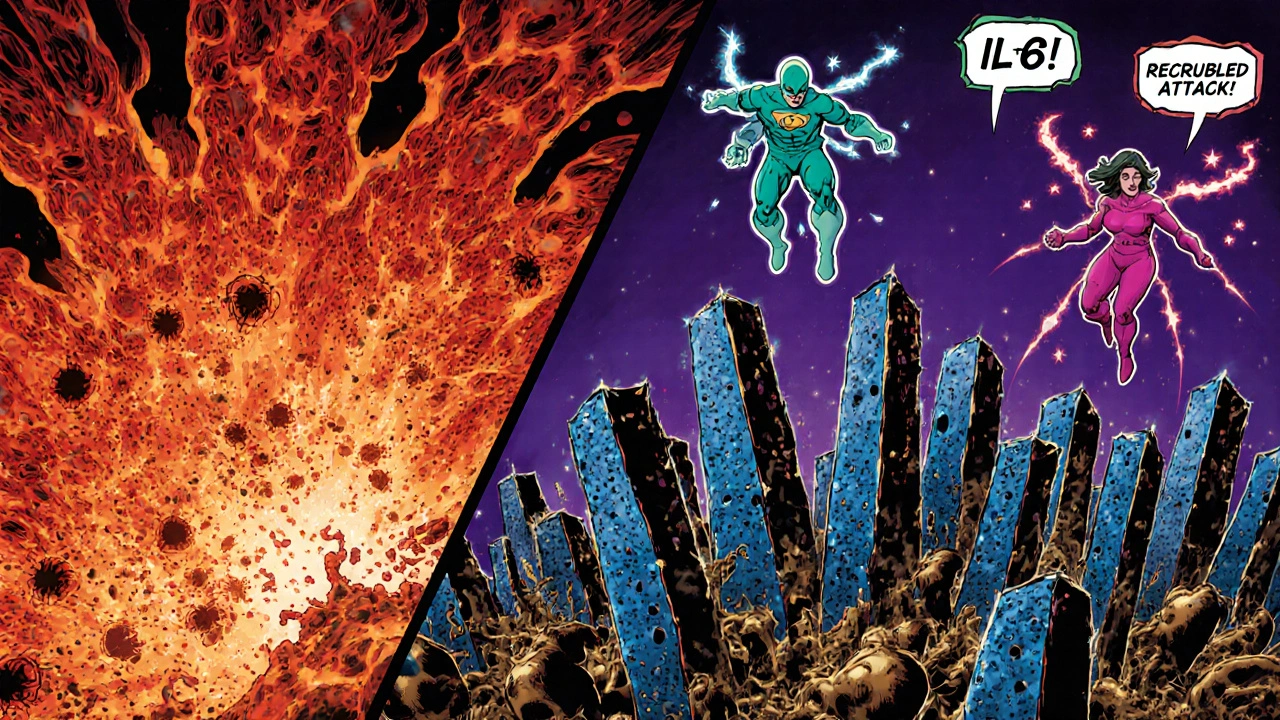
Short‑Term Immune Effects: Inflammation and Defense
Within hours of infection, the vaginal mucosa becomes inflamed. The swelling you feel is a result of increased blood flow and immune cell infiltration. Neutrophils release reactive oxygen species (ROS) that can damage the parasite but also irritate host tissue.
Simultaneously, the epithelium ramps up production of antimicrobial peptides. Studies from 2023 show a 2.5‑fold rise in β‑defensin 2 levels in infected women compared to healthy controls. While this helps control the parasite, the heightened AMP environment can also disrupt the normal balance of commensal bacteria.
Long‑Term Consequences: Microbiome Shifts and HIV Risk
If the infection lingers for weeks or months, the immune response doesn’t just stay elevated - it remodels the entire vaginal ecosystem.
One consistent finding is a drop in lactobacilli, the bacteria that keep vaginal pH low (around 3.8-4.5). A 2024 longitudinal study of 250 women showed that persistent Trichomonas vaginalis infection reduced Lactobacillus crispatus density by 70% and increased Gardnerella vaginalis by 150%.
These changes produce a higher pH, creating a more permissive environment for other pathogens. Moreover, the chronic inflammatory milieu up‑regulates CCR5 and CXCR4 receptors on CD4+ T‑cells, which HIV uses to gain entry.
Meta‑analyses from 2022‑2024 estimate that women with untreated trichomoniasis have a 2.8‑fold greater chance of acquiring HIV during heterosexual intercourse. The mechanism is twofold:
- Physical: ulceration or micro‑tears in the mucosa provide direct access.
- Biological: activated immune cells congregate at the site, offering more target cells for the virus.
Key Immune Markers: A Quick Comparison
| Marker | Healthy baseline | Infected (acute) | Infected (chronic) |
|---|---|---|---|
| IL‑1β (pg/mL) | 5±2 | 18±5 | 12±4 |
| IL‑6 (pg/mL) | 4±1 | 15±3 | 9±2 |
| TNF‑α (pg/mL) | 3±1 | 14±4 | 8±3 |
| β‑defensin 2 (ng/mL) | 0.8±0.3 | 2.0±0.5 | 1.5±0.4 |
| Lactobacillus spp. (CFU/mL) | 10⁶‑10⁷ | 10⁵‑10⁶ | 10⁴‑10⁵ |
These numbers illustrate the spike in inflammatory cytokines during the acute phase and the lingering, though lower, elevation during chronic infection. Notice the parallel dip in beneficial lactobacilli - a key factor in long‑term susceptibility.
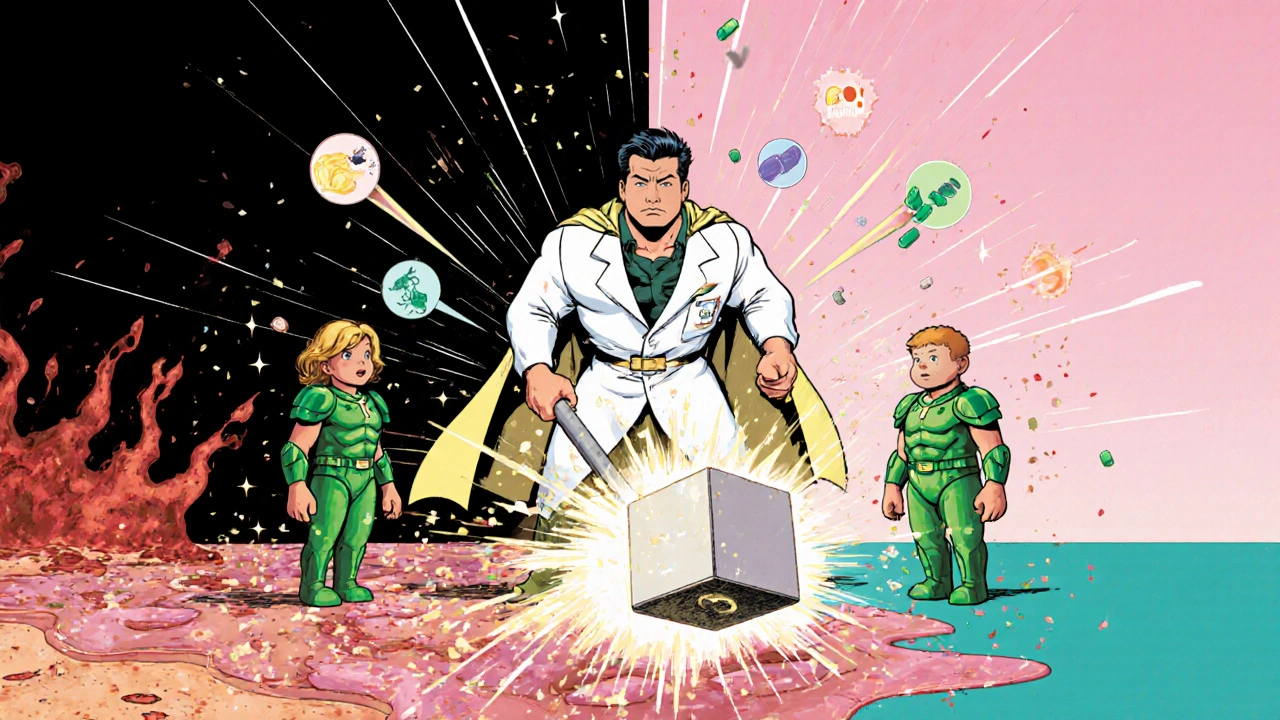
Managing the Immune Impact: Treatment and Support
Standard therapy involves a single oral dose of metronidazole (2g) or tinidazole (2g). Both drugs eradicate >95% of parasites when taken correctly. However, drug resistance is emerging in some regions, so a repeat dose or combination therapy may be required.
Beyond antibiotics, consider these immune‑friendly steps:
- Probiotics: Strains like Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 have been shown in a 2023 randomized trial to restore lactobacilli levels within four weeks post‑treatment.
- Omega‑3 fatty acids: They temper cytokine production, lowering IL‑6 and TNF‑α by roughly 20% in inflamed mucosal tissue.
- Avoid douching or scented products, which further disrupt the microbiome and can prolong inflammation.
Follow‑up testing is recommended three weeks after treatment to confirm clearance, especially for pregnant women or those with HIV risk factors.
When to See a Healthcare Provider
If you experience any of the following, schedule a visit promptly:
- Persistent itching, burning, or abnormal discharge lasting more than a week.
- Recurring infections despite treatment - this may indicate drug resistance or re‑exposure.
- Pregnancy, because untreated trichomoniasis can increase preterm birth risk.
- HIV‑positive status - regular screening is crucial, as co‑infection worsens outcomes.
The good news is that with proper treatment and microbiome support, immune markers typically return to baseline within two months.
Frequently Asked Questions
Can trichomoniasis be spread without sexual contact?
Rarely, the parasite can be transmitted from mother to newborn during vaginal delivery, leading to urinary tract infection in the infant. Otherwise, sexual activity is the primary route.
Why do some people have no symptoms?
The parasite may remain at low numbers, eliciting a mild immune response that doesn’t produce noticeable irritation. Men often have asymptomatic infections, serving as hidden carriers.
Does treating trichomoniasis fix the immune changes?
Yes, effective antibiotic therapy clears the parasite, which allows cytokine levels to fall and the vaginal microbiome to rebalance, especially when combined with probiotics.
Can trichomoniasis increase the risk of other STIs besides HIV?
The inflammatory environment and disrupted mucosal barrier also raise susceptibility to chlamydia, gonorrhea, and HPV. Screening for multiple STIs is advised after a trichomoniasis diagnosis.
Is there a vaccine in development?
Researchers are exploring recombinant proteins and DNA‑based vaccines targeting the parasite’s surface adhesins. Early‑phase trials in 2024 showed promising antibody responses, but a market‑ready vaccine is still years away.
Bottom line: trichomoniasis isn’t just a harmless irritation. It sets off a chain reaction in your immune system, reshapes the vaginal microbiome, and can open doors for more serious infections. Prompt treatment, coupled with probiotic and nutritional support, restores balance and protects your broader health.
Ragha Vema
September 7, 2025 AT 08:47Ah, the hidden puppet strings of tiny parasites! It's like the government wants us to ignore how a simple protozoan can open the floodgates for something as massive as HIV. The drama of our immune system being hijacked is insane, but we can fight back with proper meds. Stay safe, friends!
Scott Mcquain
September 9, 2025 AT 13:56It is absolutely unacceptable that someone would downplay the seriousness of trichomoniasis; it is a public health crisis!!! The data are crystal‑clear; neglect leads to higher HIV risk; therefore, treatment MUST be prioritized.
kuldeep singh sandhu
September 11, 2025 AT 19:04Well, maybe the whole alarm over trichomoniasis is just overblown, but who knows, right? Sometimes the hype is bigger than the problem.
Zac James
September 14, 2025 AT 00:13From a cultural perspective, many communities still view STIs with stigma, which can delay testing and treatment. Sharing accurate info helps break those barriers and supports public health.
Arthur Verdier
September 16, 2025 AT 05:22Oh sure, because the pharma industry totally wants you to stay infected so they can keep selling metronidazole forever. If you read the studies, the numbers are crystal‑clear: untreated trich infection boosts HIV risk by nearly threefold. Get the meds, trust the science, stop being a conspiracy nut.
Breanna Mitchell
September 18, 2025 AT 10:30You’re right, we can beat this!
Alice Witland
September 20, 2025 AT 15:39While I appreciate the enthusiasm, let’s remember that proper grammar also matters when disseminating health info – clarity prevents misunderstandings. Also, a dash of sarcasm doesn’t replace solid evidence, does it?
Chris Wiseman
September 22, 2025 AT 20:47The interplay between Trichomonas vaginalis and the host immune system is a textbook example of a pathogen turning the body's defenses into its own ally. When the parasite latches onto the vaginal epithelium, it instantly triggers pattern‑recognition receptors that unleash a cascade of pro‑inflammatory cytokines such as IL‑1β, IL‑6, and TNF‑α. This acute inflammation creates a hostile environment for the parasite but simultaneously damages the mucosal barrier, making it easier for other microbes to slip through. In the first few days of infection, neutrophils flood the site, releasing reactive oxygen species that, while attempting to kill the protozoan, also irritate host cells. The epithelium responds by producing antimicrobial peptides like β‑defensin 2, which further skews the local microbiome away from beneficial lactobacilli. Studies have repeatedly shown a sharp decline in Lactobacillus crispatus populations during persistent infection, often dropping by more than 70 percent. The resulting rise in vaginal pH creates a fertile breeding ground for opportunistic bacteria such as Gardnerella vaginalis and Atopobium vaginae. This dysbiosis is not merely a side effect; it fuels a chronic low‑grade inflammation that keeps immune activation elevated for weeks or months. Chronic activation up‑regulates CCR5 and CXCR4 receptors on resident CD4+ T cells, providing HIV with more entry points. Meta‑analyses from the past few years estimate that women harboring untreated trichomoniasis face roughly a 2.8‑fold increased odds of acquiring HIV during heterosexual intercourse. Moreover, the micro‑tears in the mucosa, both visible and subclinical, serve as physical portals for viral entry. The good news is that a single dose of metronidazole or tinidazole can clear over 95 percent of the parasites, allowing cytokine levels to fall back toward baseline. However, antibiotic treatment alone often leaves the microbiome in a fragile state, which is why adjunct probiotic therapy with strains like Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14 is strongly recommended. These probiotics not only help re‑establish a low pH but also compete with pathogenic bacteria, reducing the likelihood of reinfection and lingering inflammation. In summary, the parasite’s ability to hijack our immune response underscores the importance of early diagnosis, prompt treatment, and holistic restoration of vaginal health.
alan garcia petra
September 25, 2025 AT 01:56That long rundown was solid, bro – really breaks down why we shouldn’t ignore the symptoms. Good reminder to get checked and maybe add some yogurt‑friendly probiotics.
Allan Jovero
September 27, 2025 AT 07:04While I appreciate the supportive tone, please note that the term 'bro' is inappropriate in academic discourse and that 'yogurt‑friendly' is colloquial. A more precise recommendation would be to cite specific Lactobacillus strains and dosage.
Andy V
September 29, 2025 AT 12:13Also, the previous comment omitted the recommended follow‑up interval of three weeks post‑treatment; this detail is crucial for confirming eradication.
Sen Đá
October 1, 2025 AT 17:22Thank you for highlighting the follow‑up schedule; adhering to a three‑week test ensures that any residual infection is detected promptly, which is especially important for patients with comorbidities.
LEE DM
October 3, 2025 AT 22:30Exactly, consistent testing and timely treatment keep both the microbiome and immunity in balance.
Amy Aims
October 6, 2025 AT 03:39Love the positivity! 😊 Keep spreading the word and stay healthy!
Shaik Basha
October 8, 2025 AT 08:47yo man, totally agree, keep it real and get that checkup asap lol