
Verapamil Dosage Calculator
Verapamil Dosage Calculator
Select an indication and formulation to see dosage recommendations.
Ever wondered why a single pill can calm a racing heart, lower blood pressure, and ease chest pain? That’s the story of Verapamil, a versatile calcium channel blocker that’s been a mainstay in cardiology for decades.
Key Takeaways
- Verapamil blocks L-type calcium channels, reducing heart muscle contraction and vascular tone.
- It’s approved for hypertension, angina, and several cardiac arrhythmias such as atrial fibrillation.
- The drug is metabolized primarily by CYP3A4 and excreted unchanged via the kidneys.
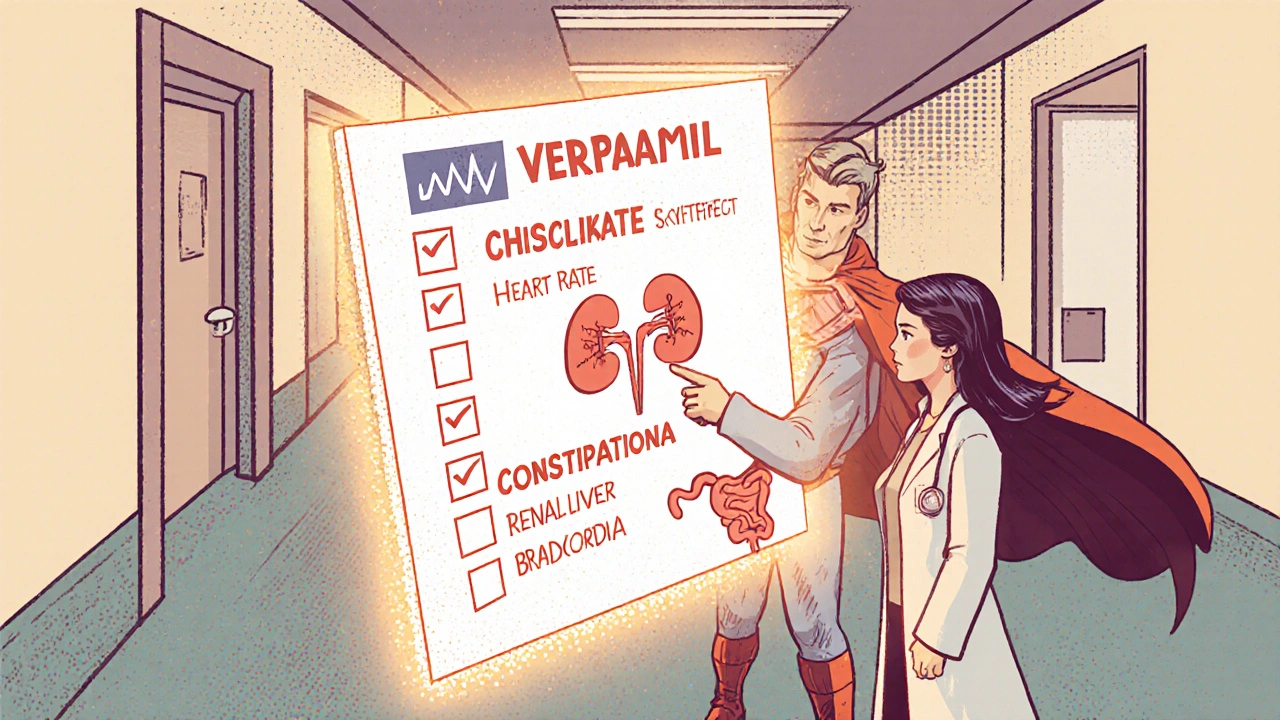
- Common side effects include constipation, dizziness, and slowed heart rate; severe risks involve heart block and heart failure.
- Drug interactions are frequent - avoid strong CYP3A4 inhibitors and be cautious with other calcium‑channel blockers.
What Is Verapamil?
Verapamil is a synthetic phenylalkylamine that belongs to the calcium channel blocker class. First approved in the early 1980s, it quickly gained traction for its dual action on cardiac muscle and vascular smooth muscle. Chemically, it is a non‑dihydropyridine (NDHP) agent, which differentiates it from the dihydropyridine family (like amlodipine) that primarily target blood vessels.
How Verapamil Works - The Mechanism
At the cellular level, verapamil binds to the α1‑subunit of L‑type calcium channels located on cardiac myocytes and smooth‑muscle cells. By inhibiting calcium influx, it reduces the force of contraction (negative inotropy) and slows conduction through the atrioventricular (AV) node (negative dromotropy). This dual effect explains why the drug lowers blood pressure while also acting as an anti‑arrhythmic.
Because the AV node relies heavily on calcium currents for depolarization, verapamil is especially effective in controlling supraventricular tachycardias and atrial fibrillation. Its impact on vascular smooth muscle leads to modest vasodilation, which contributes to its antihypertensive properties without causing the rapid heart‑rate reflex seen with many vasodilators.

Therapeutic Uses
Clinicians prescribe verapamil for three major indications:
- Hypertension: Often used when patients need both blood‑pressure control and rate control for concurrent arrhythmias.
- Angina pectoris: By decreasing myocardial oxygen demand and improving coronary blood flow.
- Atrial fibrillation and other supraventricular tachycardias: Provides rate control without the beta‑blocker‑related bronchospasm risk.
Off‑label, it may be used for migraine prophylaxis or certain cluster headaches, but those applications are less common.
Pharmacokinetics - What Happens After You Swallow It?
Absorption is rapid, with peak plasma concentrations reached in 1-2hours for immediate‑release (IR) tablets and 4-6hours for extended‑release (ER) formulations. Food modestly reduces the rate of absorption but does not significantly affect overall exposure.
Distribution is extensive; the drug is about 90% protein‑bound, mainly to albumin. Volume of distribution averages 3L/kg, reflecting its ability to penetrate cardiac tissue.
Metabolism occurs primarily in the liver via the cytochrome P450 isoenzyme CYP3A4. Approximately 30% is excreted unchanged in the urine, while the rest is eliminated as inactive metabolites. The average elimination half‑life is 3-7hours for IR and 5-9hours for ER forms.
Because verapamil is a substrate for the efflux transporter P‑glycoprotein, inhibitors of this pump (e.g., quinidine) can raise plasma levels and increase toxicity risk.
Dosage Forms & Typical Dosing
Verapamil is available as oral tablets (IR and ER), capsules, and intravenous injections. Dosing varies by indication, age, renal function, and whether the patient is on concurrent medications that affect CYP3A4.
- Hypertension: Start with 80mg IR three times daily or 120mg ER once daily. Titrate up to 240mg ER daily as needed.
- Angina: 80-120mg IR three times daily, or 180mg ER once daily. For chronic stable angina, the ER formulation offers better compliance.
- Atrial fibrillation/Rate control: 120mg IR three times daily or 240mg ER once daily. In patients with heart failure, begin at the low end and monitor closely.
- IV administration: 5-10mg over 2minutes for acute rate control, followed by a maintenance infusion of 0.1-0.2mg/kg/hr.
Always adjust the dose in renal impairment (CrCl<30mL/min) and in hepatic dysfunction, as reduced clearance can lead to accumulation.
Side Effects & Safety Concerns
While verapamil is generally well‑tolerated, its pharmacology predisposes patients to several predictable adverse events:
- Constipation: Occurs in up to 15% of users; stay hydrated and consider fiber supplements.
- Bradycardia and AV‑block: Particularly in patients with pre‑existing conduction disease; baseline ECG is essential.
- Hypotension: More common with the IR formulation and when combined with other vasodilators.
- Peripheral edema: Usually mild; dose reduction often helps.
- Heart failure exacerbation: Negative inotropic effect can worsen systolic dysfunction; avoid in severe left‑ventricular failure (NYHAIII-IV).
Rare but serious reactions include severe bradyarrhythmias, myocardial depression, and allergic skin eruptions. If a patient experiences dizziness, fainting, or a sudden drop in pulse, seek medical attention immediately.
Drug Interactions - What to Watch Out For
Verapamil’s metabolism and transport pathways make it a frequent culprit in drug‑interaction dilemmas. Key interactions include:
- Strong CYP3A4 inhibitors (ketoconazole, clarithromycin, ritonavir): Can double or triple verapamil levels, raising the risk of toxicity.
- CYP3A4 inducers (rifampin, carbamazepine, phenytoin): May reduce efficacy, requiring dose escalation.
- P‑glycoprotein inhibitors (quinidine, verapamil itself): Lead to higher plasma concentrations.
- Other calcium‑channel blockers (diltiazem, amlodipine): Additive negative inotropic and AV‑node effects; avoid co‑administration unless closely monitored.
- Beta‑blockers (metoprolol, atenolol): Can cause excessive bradycardia; dose adjustments are mandatory.
- Digoxin: Verapamil raises digoxin levels by reducing clearance; monitor serum digoxin.
Therapeutic drug monitoring isn’t routine for verapamil, but plasma level checks can be valuable when dealing with polypharmacy, especially in the elderly.
How Verapamil Stacks Up Against Similar Drugs
| Attribute | Verapamil (NDHP) | Diltiazem (NDHP) | Amlodipine (DHP) |
|---|---|---|---|
| Primary Action | Strong negative inotropy & dromotropy | Moderate negative inotropy, stronger vasodilation | Predominant vasodilation, minimal cardiac effect |
| Key Indications | Hypertension, angina, supraventricular tachycardia | Angina, rate control in AF, hypertension | Hypertension, chronic angina |
| Metabolism | CYP3A4 | CYP3A4 | CYP3A4 |
| Half‑life (ER) | 5-9h | 4-6h | 30-50h |
| Common Side Effects | Constipation, bradycardia | Headache, edema | Swelling, flushing |
Choose verapamil when rate control is a priority; pick diltiazem for a balance of heart‑rate and blood‑pressure effects; opt for amlodipine if you need a once‑daily, long‑acting antihypertensive with minimal cardiac impact.
Monitoring & Patient Tips
Effective and safe use of verapamil hinges on a few practical steps:
- Baseline ECG: Detect existing AV‑node disease or QT prolongation.
- Blood pressure & pulse checks: Verify that heart rate stays above 50bpm unless intentional pacing is used.
- Renal and liver labs: Adjust dose if creatinine clearance <30mL/min or severe hepatic impairment.
- Watch for constipation: Increase dietary fiber, fluid intake, and consider laxatives if needed.
- Review medication list regularly: Flag CYP3A4 inhibitors, other CCBs, and beta‑blockers.
Patients should never stop verapamil abruptly, especially if it’s controlling a rhythm problem; tapering reduces rebound tachycardia risk.
Frequently Asked Questions
Can I take verapamil with a beta‑blocker?
Yes, but only under close medical supervision. The combination can cause excessive bradycardia or AV‑block. Doctors usually start both drugs at low doses and monitor heart rate and blood pressure.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one-don’t double up, as high plasma levels can cause dizziness or fainting.
Is verapamil safe during pregnancy?
The drug is classified as Category C in the US, meaning risk cannot be ruled out. It should only be used if the potential benefit outweighs the risk, and always under specialist guidance.
Why do I feel constipated after starting verapamil?
Verapamil reduces smooth‑muscle activity in the gastrointestinal tract, slowing transit. Increasing water intake, fiber, and gentle exercise can help. If constipation becomes severe, ask your doctor about a stool softener.
Can verapamil cause heart failure?
In patients with existing systolic dysfunction, the negative inotropic effect can worsen heart failure. For those with preserved ejection fraction, it’s generally safer, but close monitoring is still required.
Understanding the Verapamil pharmacology equips you to use the drug wisely, spot problems early, and talk intelligently with your healthcare team. Whether you’re a patient, a caregiver, or a clinician, the key is to respect its powerful cardiac actions while managing its quirks.
Jacob Hamblin
October 11, 2025 AT 09:35Verapamil’s dual action can be a bit confusing at first, but the key point is that it softens both the heart’s contractility and the vascular tone. By blocking L‑type calcium channels it reduces the force of contraction and slows AV‑node conduction, which explains its use in hypertension, angina, and supraventricular arrhythmias. If you’re starting a patient on the immediate‑release form, 80 mg three times daily is a gentle entry point, while the extended‑release version often begins at 120 mg once daily. Always keep an eye on renal function; a CrCl below 30 mL/min usually calls for a 50 % dose reduction. I hope this helps clear up the basics, and feel free to share any experiences you’ve had with dose titration.
Herman Rochelle
October 24, 2025 AT 07:35When you’re coaching a newcomer through the dosage calculator, remind them that the “weight” input only matters for the IV scenario – the oral forms rely on renal function and indication. Start low, watch blood pressure and heart rate, then titrate up in small increments; that’s the safest route. Avoid pairing strong CYP3A4 inhibitors like ketoconazole without adjusting the dose, because plasma levels can climb quickly. Keep a notebook of any constipation or dizziness, as those are the most common side effects. You’ve got this, and the step‑by‑step approach will keep things steady.
Stanley Platt
November 6, 2025 AT 04:35Verapamil, as a non‑dihydropyridine calcium‑channel blocker, exerts its pharmacologic influence primarily upon cardiac myocytes and vascular smooth muscle; consequently, it produces negative inotropy, negative dromotropy, and modest vasodilation. Its metabolism via CYP3A4, coupled with approximately 30 % renal excretion, necessitates vigilance when co‑administered with potent inhibitors or in patients with compromised renal clearance. Dose‑adjustment guidelines recommend a 50 % reduction for CrCl < 30 mL/min in the immediate‑release formulation, whereas the extended‑release preparation often tolerates a slightly higher ceiling. Clinical vigilance remains paramount, especially regarding bradycardia or heart block in susceptible individuals. Stay attentive, and the therapy can be both effective and safe. :)
Alice Settineri
November 19, 2025 AT 02:35Alright, let’s cut to the chase – Verapamil is basically the Swiss‑army knife of cardio drugs, juggling blood pressure, chest pain, and rogue heartbeats all at once. If you drop the IR 80 mg TID on a hypertensive patient, you’re giving the heart a gentle “take it easy” nudge, while the ER 120 mg QD ramps up the convenience factor without sacrificing potency. The drug’s love‑hate relationship with the liver (CYP3A4) means you better watch out for booze, grapefruit, and those nasty antifungals that love to hog the enzyme. And hey, if your patient starts complaining about constipation, don’t just shrug – that’s a textbook side‑effect screaming for a tweak in fiber intake or a dose reduction. Bottom line: respect the dosing calculator, respect the kidneys, and you’ll keep the heart humming like a well‑tuned jazz band.
Dawson Turcott
December 2, 2025 AT 00:35Oh great, another calcium blocker, just what we needed 🙄.
Alex Jhonson
December 14, 2025 AT 22:35Verapamil’s mechanism is pretty straight‑forward – it blocks L‑type calcium channels, which calms the heart and relaxes blood vessels. The IR tablets start at 80 mg three times a day, while the ER tablets usually start at 120 mg once daily. If the patient has a low CrCl, you should probably cut the dose in half – that’s just good practice. Also, watch out for drug interactions with strong CYP3A4 inhibitors, they can raise levels and cause bradycardia. Hope this helps, let me know if you need any more details.
Katheryn Cochrane
December 27, 2025 AT 20:35Reading this article feels like watching a bland PowerPoint presentation on a drug that has been around since the 80s – nothing groundbreaking, just a re‑hash of old textbooks. The dosage tables are useful, sure, but the writer neglects to mention the real‑world nightmare of managing constipation in elderly patients, which often leads to hospitalization. Also, the warning about heart block is buried under a generic “critical warning” blurb, when in fact it should be front‑and‑center for anyone prescribing to a patient with pre‑existing conduction disease. In short, the piece is informative but dangerously superficial; clinicians need more than a checklist – they need context, nuance, and a reminder that Verapamil isn’t a magic bullet.
Michael Coakley
January 9, 2026 AT 18:35Philosophically speaking, Verapamil demonstrates the paradox of medicine: we tame the heart’s rhythm by throttling calcium, yet we risk slowing the very life force we aim to protect. It's a sleek little molecule that masquerades as a harmless tablet while it can usher in bradycardia if you aren’t careful. The IR dosing feels like a lesson in modesty – 80 mg three times a day, like a cautious whisper. The ER version shouts “convenience,” but at the cost of a longer half‑life and potential accumulation. So, next time you pop a pill, remember that each dose carries a tiny philosophical debate between efficacy and safety. Cool, right?
ADETUNJI ADEPOJU
January 22, 2026 AT 16:35From a pharmacokinetic standpoint, verapamil exemplifies a substrate‑inhibitor duality within the CYP3A4 enzymatic framework, thereby imposing a considerable ontogenetic burden on co‑administered agents with overlapping metabolic pathways. The clinician, therefore, must execute a regimen of vigilant therapeutic drug monitoring, especially when confronting polypharmacy scenarios rife with macrolide antibiotics or azole antifungals, which function as potent enzyme inhibitors. Moreover, the drug’s classification as a P‑glycoprotein substrate introduces an additional vector of variability in bioavailability, necessitating dose recalibration in the context of concomitant P‑gp modulators. While the literature extols its efficacy in rate control, the pragmatic implications of its negative inotropic profile cannot be understated, particularly in heart‑failure cohorts where afterload reduction may precipitate hemodynamic compromise.
Janae Johnson
February 4, 2026 AT 14:35Interesting read, though I must respectfully disagree with the emphasis on Verapamil as a first‑line agent for hypertension in the modern era. Current guidelines tend to favor ACE inhibitors or ARBs as initial therapy, reserving calcium‑channel blockers for specific populations. While the drug certainly has its place, the article glosses over the comparative risk‑benefit profile that newer agents offer, especially regarding metabolic side effects. Still, the mechanistic explanation is sound, and the dosage calculator is a handy tool for those who still prescribe it. Just remember that clinical practice evolves, and what was once “standard” may now be “selective.”
Kayla Charles
February 17, 2026 AT 12:35Verapamil, first introduced in the early 1980s, has endured as a cornerstone in cardiovascular therapeutics, largely because of its unique ability to simultaneously modulate myocardial contractility and vascular tone, a duality that few agents can claim.
The drug’s pharmacodynamic profile is rooted in its high affinity for L‑type calcium channels, which are abundant in both cardiac myocytes and smooth‑muscle cells, thereby reducing intracellular calcium influx and attenuating the force of contraction.
This negative inotropic effect translates clinically into lower myocardial oxygen consumption, a benefit that is especially valuable in patients suffering from angina pectoris.
Equally important is the drug’s negative dromotropic action; by slowing conduction through the atrioventricular node, Verapamil provides reliable rate control for atrial fibrillation and other supraventricular tachyarrhythmias.
When prescribing, clinicians often start with an immediate‑release formulation of 80 mg taken three times daily for hypertension, appreciating the flexibility to titrate in modest increments while monitoring blood pressure and heart rate.
For patients who prioritize dosing convenience, the extended‑release tablet offers a once‑daily option, typically beginning at 120 mg and potentially escalating to 240 mg based on therapeutic response and tolerability.
Renal function plays a pivotal role in dose adjustment; a creatinine clearance below 30 mL/min generally warrants a 50 % reduction, irrespective of the formulation, to mitigate the risk of drug accumulation and adverse events.
Pharmacokinetically, Verapamil exhibits a bioavailability of roughly 20 % for the immediate‑release form, with food modestly slowing absorption but not significantly altering the area under the curve, a fact that allows for flexible dosing with respect to meals.
The drug’s metabolism is predominantly hepatic, mediated by the cytochrome P450 enzyme CYP3A4, which introduces a substantial potential for drug‑drug interactions, particularly with strong inhibitors such as ketoconazole, erythromycin, or certain HIV protease inhibitors.
In such scenarios, clinicians must either reduce the Verapamil dose or consider alternative rate‑control agents to avoid excessive plasma concentrations that could precipitate bradycardia or advanced heart block.
Beyond its cardiovascular applications, off‑label uses of Verapamil have emerged in migraine prophylaxis and even cluster headache management, reflecting its broader neuromodulatory effects, although these indications remain less substantiated in large‑scale trials.
Adverse effects remain relatively predictable, with constipation being the most common gastrointestinal complaint, followed by dizziness, fatigue, and flushing; patients should be counseled on dietary fiber intake and hydration to alleviate these symptoms.
Serious complications, though rare, include severe bradyarrhythmias, atrioventricular block, and exacerbation of heart failure, especially in individuals with pre‑existing reduced ejection fraction, underscoring the necessity for regular electrocardiographic monitoring during dose titration.
Clinical guidelines advise careful assessment of baseline cardiac conduction before initiating therapy, and any new onset of syncope or marked bradycardia should prompt immediate evaluation and possible discontinuation of the drug.
In summary, Verapamil remains a versatile and effective agent when used judiciously, with its benefits heavily contingent upon individualized dosing, vigilant monitoring for drug interactions, and a proactive approach to managing its well‑characterized side‑effect profile.