Wilson’s disease isn’t something you hear about every day. But if you’ve had unexplained liver problems, tremors, or trouble speaking-especially as a teenager or young adult-it might be the hidden cause. This rare genetic disorder doesn’t attack because of bad habits or poor diet. It’s built into your DNA. And if left untreated, it can destroy your liver, scramble your brain, and even kill you. The good news? With the right treatment, most people live full, normal lives. The key is understanding how copper builds up in your body-and how to safely remove it.
What Happens When Your Body Can’t Get Rid of Copper
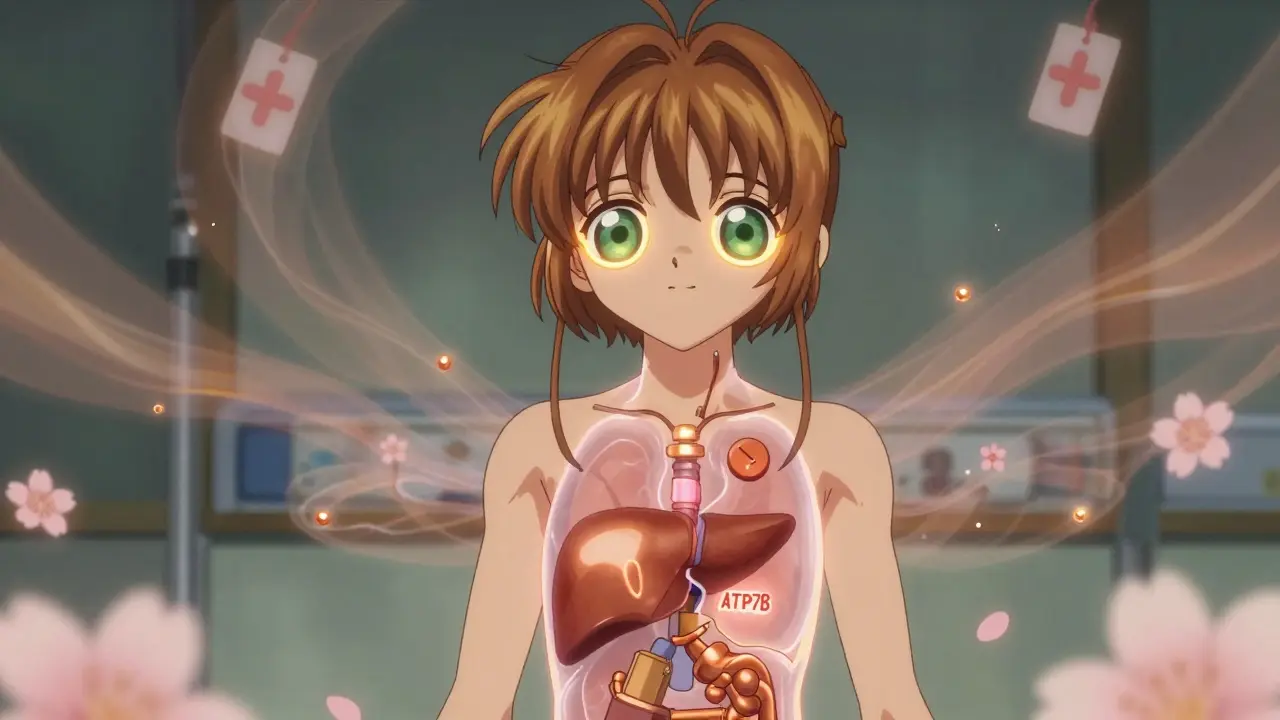
Every person needs a little copper. It helps make red blood cells, keeps nerves working, and supports your immune system. But your body doesn’t make copper-it gets it from food. Normally, your liver takes in copper from your gut, uses what it needs, and pushes the rest out through bile into your intestines. That’s where the ATP7B gene comes in. It’s the blueprint for a protein that acts like a copper pump in liver cells. In Wilson’s disease, this gene is broken. The pump doesn’t work. Copper piles up.
At first, your liver tries to save itself. It locks copper away in proteins like metallothionein. But after years of this slow buildup, the storage runs out. Copper leaks into your bloodstream as free copper-the dangerous kind. It doesn’t bind to ceruloplasmin like it should. Instead, it travels to your brain, kidneys, and eyes. In the brain, it targets the basal ganglia, the area that controls movement. That’s why people with Wilson’s disease often develop tremors, stiffness, or trouble swallowing. In the eyes, copper forms a golden-brown ring around the iris called a Kayser-Fleischer ring. It’s invisible to the naked eye, but doctors spot it with a simple slit-lamp exam.
What makes Wilson’s disease tricky is that symptoms can look like almost anything else. Liver enzyme spikes? Could be fatty liver. Mood swings and depression? Maybe stress. Tremors? Parkinson’s. That’s why it often takes years to diagnose. The average delay is over two years. By then, damage might already be done.
How Doctors Diagnose Wilson’s Disease
There’s no single test that confirms Wilson’s disease. Doctors piece it together like a puzzle. First, they check your blood. Low ceruloplasmin-a protein that carries copper-is a big red flag. Normal levels are 20-50 mg/dL. In Wilson’s, they’re often below 20. But here’s the catch: kids under five and pregnant women can have naturally low ceruloplasmin. So it’s not foolproof.
The next clue? Urine. A 24-hour urine copper test measures how much copper your body is dumping. Normal is under 40 micrograms. In Wilson’s, it’s usually over 100-sometimes even 300 or more. But in people with neurological symptoms, this number can be misleading. That’s why doctors also look at free copper in your blood. Anything above 10 μg/dL is suspicious.
A slit-lamp eye exam is quick and painless. If you see that copper ring, it’s a major clue. And if you have a family history of Wilson’s? That’s another strong indicator. Genetic testing for ATP7B mutations is now part of the diagnostic toolkit. If you have two faulty copies of the gene, the diagnosis is confirmed. The 2023 updated guidelines even let a positive gene test count as four points in the diagnostic scoring system-enough on its own to confirm the disease.
Chelation Therapy: How It Works and Why It’s Necessary
Once Wilson’s disease is confirmed, treatment starts fast. The goal isn’t just to lower copper-it’s to remove the toxic buildup without making you copper-deficient. That’s where chelation therapy comes in.
Chelators are drugs that grab onto copper like a magnet and carry it out through your urine. The two main ones are D-penicillamine and trientine. D-penicillamine has been around since the 1950s. It’s cheap-about $300 a month in the U.S.-but it comes with a nasty side effect: up to half of patients get worse before they get better. Within weeks, tremors can spike, speech gets slurred, and muscle control worsens. That’s because the chelator pulls copper out of the liver so fast that it floods the brain temporarily.
To counter this, doctors often add zinc. Zinc doesn’t remove copper. It blocks your gut from absorbing it. Taking 50 mg of elemental zinc three times a day, on an empty stomach, helps stabilize things. It’s a safety net.
Trientine is the alternative. It’s less likely to cause neurological worsening and has fewer side effects. But it costs nearly six times as much-around $1,850 a month. That’s a huge barrier, especially without good insurance. In Europe, trientine is used more often. In the U.S., cost still pushes many toward D-penicillamine.

What Happens After the First Wave of Treatment
Chelation isn’t a cure. It’s a lifelong process. After six to twelve months, most patients switch from chelators to maintenance therapy. That’s where zinc acetate takes over. It’s not as aggressive, but it’s safer for long-term use. Zinc keeps copper from entering your bloodstream by triggering your gut to make metallothionein-a protein that traps copper and flushes it out in stool.
Monitoring is critical. Every three months, you’ll need blood tests to check liver enzymes, free copper, and ceruloplasmin. Every six months, a 24-hour urine test tells your doctor if you’re excreting enough copper. The target? Between 200 and 500 micrograms per day. Too low, and you risk copper deficiency. Too high, and you’re not controlling the disease.
Patients who stick to this routine live just as long as anyone else. But missing doses? That’s dangerous. One study found 35% of people skip medication at least sometimes. Side effects like nausea, metallic taste, or skin rashes make it hard. One patient on Reddit said, “I’d take my pill, then throw up. I’d forget again the next day.”
Dietary Changes and Real-Life Challenges
Medication alone isn’t enough. You also have to cut back on copper-rich foods. That means avoiding shellfish, organ meats, mushrooms, nuts, chocolate, and even some drinking water from copper pipes. The goal is under 1 milligram of copper per day. Sounds simple? Try eating a balanced diet with that limit. Many patients struggle with protein intake, iron deficiency, or just plain boredom with food.
One woman in Bristol told her doctor she’d given up almonds and lentils, but still felt tired. Turns out, she was eating fortified breakfast cereal-each bowl had 1.2 mg of copper. No one told her to check labels. Diet changes need to be personalized, not just handed out as a list.

New Treatments on the Horizon
The field is changing. In 2023, a new drug called CLN-1357 showed up in clinical trials. It’s a polymer that binds copper in the blood without crossing into the brain. That means it can lower copper without triggering neurological worsening. Early results showed an 82% drop in free copper in just 12 weeks.
Another promising drug, WTX101, targets the brain directly. It’s a modified version of tetrathiomolybdate, which crosses the blood-brain barrier better than older drugs. In a 2022 trial, it prevented neurological decline in 91% of patients-far better than trientine’s 72%.
And then there’s gene therapy. Researchers are testing a virus that delivers a working copy of the ATP7B gene into liver cells. Early trials in six patients showed no serious side effects. It’s still experimental, but if it works, it could one day cure Wilson’s disease instead of just managing it.
Why This Matters Beyond the Diagnosis
Wilson’s disease is rare. Only 1 in 30,000 people have it. But its story is a powerful one. It shows how a single broken gene can lead to organ failure-and how science can turn that around. It’s not just about copper. It’s about early detection, patient education, and access to care. In low-income countries, people wait over five years for a diagnosis. Many die before treatment even starts.
For families with a history of Wilson’s, genetic testing for siblings and children is life-saving. A simple blood test can catch it before symptoms appear. And if caught early, some people never need chelation at all-zinc alone can keep copper levels safe.
Wilson’s disease isn’t a death sentence. It’s a condition that demands attention, consistency, and care. But with the right tools, it’s manageable. The real challenge isn’t the science. It’s making sure everyone who needs help gets it-before the liver fails, before the tremors start, before it’s too late.
Can Wilson’s disease be cured?
There’s no cure yet, but with lifelong treatment, Wilson’s disease can be controlled. Most people who stick to chelation or zinc therapy, follow dietary advice, and get regular monitoring live normal lifespans. Gene therapy is being tested and may offer a true cure in the future.
Is Wilson’s disease inherited?
Yes. It’s an autosomal recessive disorder, meaning you need to inherit two faulty copies of the ATP7B gene-one from each parent. If you have only one copy, you’re a carrier and won’t develop the disease, but you can pass it on. If both parents are carriers, each child has a 25% chance of having Wilson’s disease.
Why does D-penicillamine make symptoms worse at first?
D-penicillamine pulls copper out of the liver quickly. That copper enters the bloodstream and can temporarily flood the brain, worsening neurological symptoms like tremors or speech problems. This happens in 20-50% of patients. Doctors often add zinc or switch to trientine to avoid this.
Can you outgrow Wilson’s disease?
No. Wilson’s disease is genetic and lifelong. Even if you feel fine after years of treatment, stopping medication will cause copper to build up again. Lifelong therapy and monitoring are essential.
How do you know if your treatment is working?
Your doctor will track your 24-hour urinary copper (target: 200-500 μg/day), serum free copper (below 10 μg/dL), and liver enzymes. Improvement in symptoms like tremors or fatigue also signals progress. Blood and urine tests every 3-6 months are standard.
Are there foods I should avoid completely?
Yes. Avoid shellfish (like oysters and crab), organ meats (liver, kidney), mushrooms, nuts (especially cashews and Brazil nuts), chocolate, soy products, and foods cooked in copper cookware. Check labels on fortified cereals and multivitamins-they often contain copper. A registered dietitian can help you plan safe meals.
Can Wilson’s disease affect your mental health?
Yes. Copper buildup in the brain can cause depression, anxiety, mood swings, and even psychosis. Some patients are misdiagnosed with psychiatric disorders before the real cause is found. Treating the copper overload often improves mental symptoms, but counseling or medication may also be needed.
What if I can’t afford the medication?
D-penicillamine is the most affordable option at around $300/month. Many pharmaceutical companies offer patient assistance programs. In the U.S., nonprofits like the Wilson Disease Association help with drug access. Talk to your doctor-there are often ways to reduce costs or get free medication.
Hayley Ash
December 30, 2025 AT 15:07kelly tracy
January 1, 2026 AT 04:34Henry Ward
January 3, 2026 AT 04:15Nadia Spira
January 3, 2026 AT 15:58Colin L
January 5, 2026 AT 00:07Shae Chapman
January 5, 2026 AT 09:50Joseph Corry
January 7, 2026 AT 00:24srishti Jain
January 7, 2026 AT 20:03Cheyenne Sims
January 8, 2026 AT 00:03