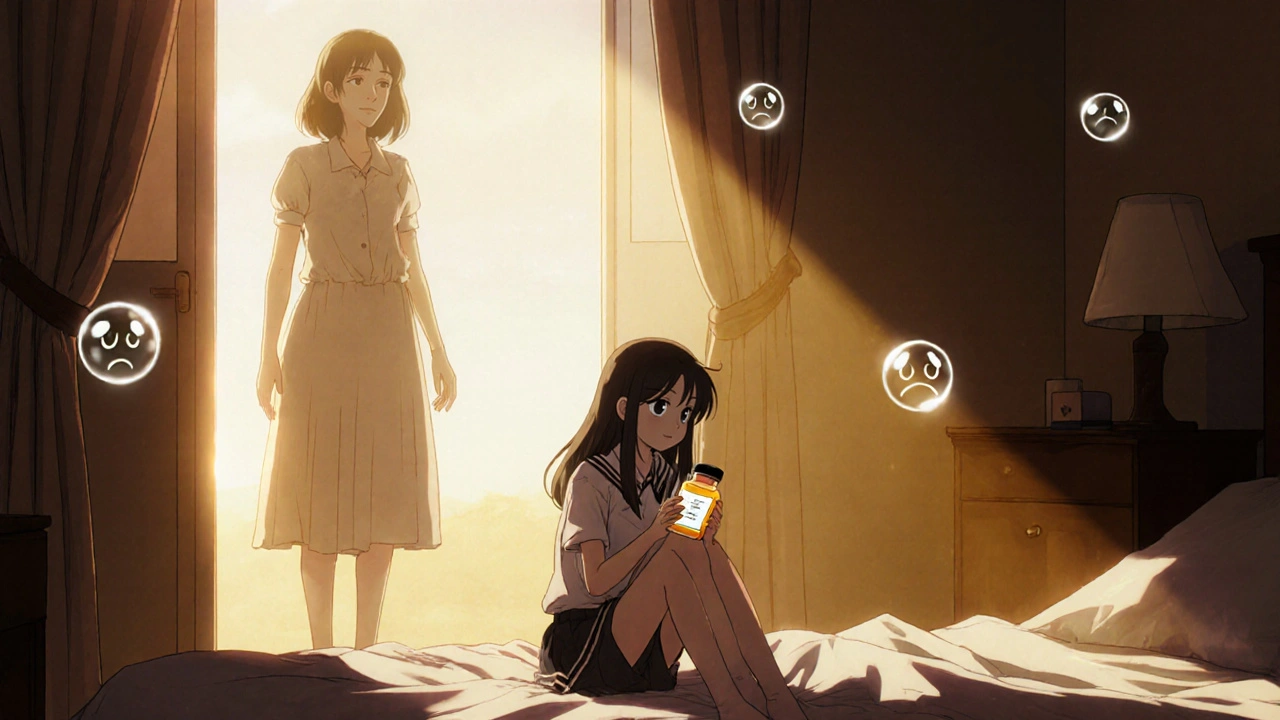
When your teenager starts showing signs of deep sadness, loss of interest in friends, or sudden silence at the dinner table, the last thing you want is to make things worse by giving them medication. But what if the very drug meant to help could also push them closer to danger? That’s the reality behind the black box warning on antidepressants for children and teens - a warning so serious it’s printed in bold black borders on every prescription bottle in the U.S.
What the Black Box Warning Actually Says
The U.S. Food and Drug Administration (FDA) added the black box warning to all antidepressants in January 2005 after reviewing data from 24 clinical trials involving over 4,400 young patients. The message is clear: antidepressants may increase the risk of suicidal thoughts and behaviors in kids and adolescents under 18. In May 2007, that warning was extended to young adults up to age 24.
The data showed that about 4% of kids taking antidepressants had suicidal thoughts or behaviors during the first few months of treatment, compared to 2% on placebo. That’s a doubling of risk - but here’s what most people miss: no child in those trials died by suicide. The warning was based on self-reported thoughts, behaviors like self-harm, or hospitalizations for worsening depression - not completed suicides.
The warning requires manufacturers to include this exact language on the packaging: “Antidepressants increase the risk of suicidal thinking and behavior (suicidality) in children and adolescents with major depressive disorder and other psychiatric disorders.” It also demands that pharmacists hand out a patient guide - called a MedGuide - with every refill, explaining the risk in plain language.
Why the Warning Was Introduced
The FDA acted because they saw a pattern. In controlled studies, a small but consistent number of young people on antidepressants began reporting more frequent thoughts of death or self-harm, especially in the first four to six weeks after starting treatment. The agency believed that if doctors and parents knew this risk existed, they could monitor kids more closely - check in weekly, watch for agitation or withdrawal, and act fast if things turned dangerous.
It made sense on paper. If you’re treating depression, you want to reduce harm. And the warning was meant to be a safety net - not a reason to avoid treatment, but a reason to treat smarter.
What Happened After the Warning Went Live
But things didn’t go as planned.
Instead of more careful monitoring, many families and doctors chose to avoid antidepressants altogether. A 2023 study from Harvard Pilgrim Health Care Institute found that within two years of the 2005 warning, antidepressant prescriptions for teens dropped by 31%. That’s over a million fewer prescriptions a year. By 2007, after the warning expanded to young adults, prescriptions for 20- to 24-year-olds fell another 24.5%.
Meanwhile, depression diagnoses in teens were going up - not down. The National Survey on Drug Use and Health showed a 14.3% increase in diagnosed depression among 12- to 17-year-olds between 2003 and 2007. More kids needed help. Fewer were getting it.
The result? Suicide rates rose. CDC data shows that from 2003 to 2007, suicide deaths among 10- to 19-year-olds jumped 75% - from 2.0 to 3.5 per 100,000. The same period saw a 21.7% spike in psychotropic drug poisonings - a common proxy for suicide attempts - among teens. For young adults, the increase was even steeper: 33.7%.
Researchers found something else: the rise in suicide attempts and deaths happened mostly in groups targeted by the warning. Adults over 25, who weren’t affected by the warning, didn’t show the same trend. That suggests the warning didn’t just change prescribing habits - it changed outcomes.

The Doctor’s Dilemma
For child psychiatrists, the warning turned every appointment into a risk assessment.
A 2019 survey of 1,200 child psychiatrists found that 87% said it was harder to prescribe antidepressants after the warning. Parents were scared. Many refused treatment outright. One parent told a doctor, “I’d rather see my child suffer than risk them killing themselves.”
Doctors now spend an extra 15 minutes per visit explaining the warning, filling out consent forms, and calming fears. The average time spent on this alone jumped from 8 minutes to over 22 minutes per patient. And even then, only 37% of teens received the recommended weekly monitoring during the first month of treatment - and in rural areas, that number dropped to 22%.
“We’re not treating depression anymore,” one psychiatrist told a researcher. “We’re managing fear.”
What the Evidence Really Shows
The original clinical trials showed a small increase in suicidal thoughts - but no deaths. The real-world data shows a sharp rise in deaths and attempts after prescriptions dropped.
Dr. Stephen Soumerai, lead author of the 2023 Health Affairs review, put it bluntly: “The consistency in observed harms and absence of observed benefits after the Black-Box Warnings indicate this is not a coincidence.”
Studies in Sweden found that after the warning, more teens died by suicide - not fewer. Researchers tracked 845 suicides between 1992 and 2010 and found that the number of deaths rose after prescriptions fell. The same pattern showed up in Canada and Australia, though less dramatically.
Meanwhile, countries like the UK and those in the European Union never issued a black box warning. Their youth suicide rates didn’t spike the same way. In fact, some saw small declines.
That’s not to say antidepressants are risk-free. They aren’t. But the warning may have done more harm than good by scaring people away from a treatment that, for many, is life-saving.

What Parents Are Saying
On Reddit’s r/mentalhealth, a thread from late 2022 asking “Should I be worried about the black box warning?” got 287 comments. Two-thirds said they were too scared to give their child antidepressants. One wrote: “I cried reading the warning. I thought I was choosing between two bad options.”
But nearly a third said they went ahead anyway - and were glad they did. A 2021 survey by the National Alliance on Mental Illness found that 67% of families who used antidepressants under careful supervision saw improvement. One mother said, “The warning made us watch closer. We noticed when she was getting worse - and we got help before it got worse.”
On HealthUnlocked, a depression support forum, 74% of parents said they delayed or refused treatment because of the warning. But among those who did treat their child, 82% said their child’s mood improved within three months.
What You Should Do Now
Here’s the bottom line: the black box warning is real. But so is the risk of untreated depression. Left alone, depression in teens can lead to school failure, substance abuse, self-harm, and suicide.
If your child is struggling:
- Don’t panic. The warning is about risk, not inevitability.
- Ask your doctor: “What’s the evidence that this medication will help my child?” and “What’s the plan for monitoring?”
- Insist on weekly check-ins during the first month. Call the doctor if your child becomes agitated, withdrawn, or talks about death.
- Don’t stop medication suddenly. Withdrawal can make depression worse.
- Combine medication with therapy. CBT and other talk therapies are proven to help - and work better with medication than alone.
There’s no perfect answer. But the best choice isn’t always the safest one - it’s the one that gives your child the best chance to get better.
The Future of the Warning
As of late 2023, the FDA is reviewing the evidence again. In June 2022, the American College of Neuropsychopharmacology called for a reevaluation. Pharmaceutical companies like Eli Lilly and Pfizer have asked the FDA to change the warning language to better reflect benefit-risk balance.
Meanwhile, researchers at the National Institute of Mental Health are working on tools to predict which teens are most at risk - not just from the medication, but from suicide itself. The goal? Replace the blanket warning with smarter, personalized guidance.
Until then, the black box remains. But the conversation is changing. More doctors are pushing back. More parents are asking questions. And more families are realizing: sometimes, the greatest risk isn’t the pill - it’s doing nothing at all.
Ravi Kumar Gupta
November 23, 2025 AT 21:54Man, this black box warning is straight-up cultural colonialism. In India, we don't have the luxury of overthinking meds like this. If your kid is silent at dinner, you give them medicine, not a therapy session. We've seen depression turn into suicide faster than you can say 'FDA'. This warning saved no one - it just scared parents into letting their kids drown in silence.
Rahul Kanakarajan
November 24, 2025 AT 18:42Wow. So you're saying the FDA caused a suicide epidemic? That's a bold claim. Where's your control group? Did you account for social media? Phone addiction? School pressure? You're blaming a warning label like it's a villain in a Marvel movie. Meanwhile, kids are getting antidepressants like candy and no one's checking if they're even diagnosed right.
New Yorkers
November 25, 2025 AT 06:49Look, I live in NYC. I've seen kids on Zoloft since they were 13. The black box? It's a joke. The real problem is that parents don't know how to talk to their kids anymore. They see 'suicidal ideation' on a label and panic. But if you actually sit down with your teen, listen without fixing, and pair meds with real therapy - it works. The warning didn't kill kids. Indifference did.
David Cunningham
November 25, 2025 AT 20:10Down under we had the same warning, but our docs just kept prescribing and added mandatory follow-ups. Suicide rates didn't spike like in the US. Maybe it's not the drug - it's how we freak out about it. We treat mental health like it's a bomb you can't touch. It's not. It's a broken leg. You fix it, you don't hide it.
luke young
November 26, 2025 AT 16:03Just want to say I appreciate how balanced this post is. My cousin was on SSRIs after her dad died, and the black box scared us at first. But we did weekly check-ins, got her into CBT, and within 6 weeks she was laughing again. It's not about avoiding risk - it's about managing it with love and attention. The warning is a tool, not a stop sign.
james lucas
November 26, 2025 AT 20:56ok so like i read this whole thing and honestly i think the fda just kinda panicked and made this warning without realizing how many people would just stop giving meds altogether. like yeah maybe 4% get more suicidal thoughts but like 70% of the kids who actually got the meds got better and stopped thinking about killing themselves. so why are we acting like the meds are the problem? the problem is we don't have enough therapists, we don't have enough time to monitor, and we're too scared to do anything. so we just hide behind a black box like it's a magic shield. it's not. it's just a sign that says 'you're on your own now'.
Jessica Correa
November 28, 2025 AT 05:11I'm a mom of a 15-year-old who went from crying every night to playing guitar again after 6 weeks on fluoxetine. The black box made me nervous but we talked to the doctor every week and watched for changes. I'm not saying it's perfect but saying no meds because of fear is like saying no insulin because of side effects. Depression kills. The pill doesn't. The silence does.
manish chaturvedi
November 29, 2025 AT 20:05As a physician from India, I must say this is a well-researched and thoughtful analysis. In our context, stigma prevents many from seeking help at all. The black box warning, while well-intentioned, has inadvertently reinforced the idea that depression is something to be feared rather than treated. We must remember: the goal of medicine is not to eliminate all risk, but to maximize benefit. The data shows that, in practice, withholding treatment causes more harm than the medication itself.
Nikhil Chaurasia
November 30, 2025 AT 07:09I understand the fear. My sister took antidepressants and became distant for a while. We didn't know if it was the medicine or her depression worsening. We waited. We watched. We cried. But we didn't stop. The black box didn't scare us - the thought of losing her did. I'm not here to say it's easy. Just that sometimes, the hardest choice is the right one.
Holly Schumacher
December 1, 2025 AT 18:18