Antidepressant Monitoring: What You Need to Track and Why It Matters
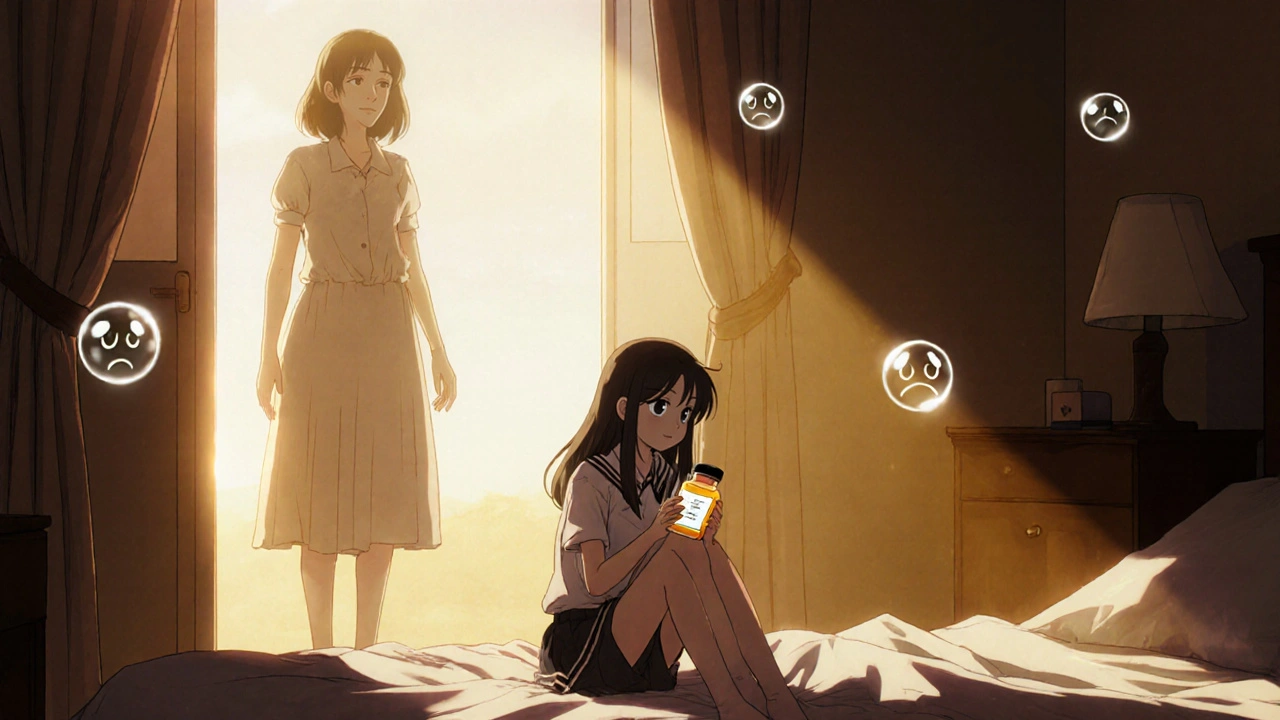
When you start taking an antidepressant, a medication used to treat depression, anxiety, and other mood disorders by balancing brain chemicals. Also known as antidepressive agents, these drugs aren’t one-size-fits-all—what works for one person might cause side effects or even reduce effectiveness in another. That’s why antidepressant monitoring isn’t optional. It’s the quiet, ongoing check-in that keeps treatment safe and working.
Monitoring means more than just showing up for a yearly appointment. It’s tracking changes in your mood, sleep, energy, and even physical symptoms like nausea or dizziness. It’s noticing if your anxiety spikes before your next dose, or if you feel emotionally numb after a few weeks. It’s asking your doctor about interactions—like how SSRIs, a common class of antidepressants that increase serotonin levels. Also known as selective serotonin reuptake inhibitors, they’re widely used but can interfere with other drugs like tamoxifen and affect breast cancer outcomes. It’s knowing that drug interactions, when two or more medications affect each other’s behavior in the body. Also known as medication clashes, they can be silent and dangerous—like how cimetidine can make heart rhythms unstable when mixed with other pills.
Some people stop their antidepressants because they feel worse before they feel better. Others switch meds without telling their doctor, thinking the new one is better. But without monitoring, you’re flying blind. You might miss early signs of serotonin syndrome, or not realize your sleep problems are tied to the timing of your dose. Even the placebo effect, when belief in a treatment changes how you feel, even if the drug has no active chemical impact. Also known as expectation-driven response, it can mask real side effects or make you think a generic isn’t working—and that’s why tracking real symptoms matters more than how you think you should feel.
You’re not just taking a pill. You’re managing a system. Your brain, your body, your other meds, your lifestyle—they all connect. That’s why monitoring isn’t about checking a box. It’s about catching what’s hidden: a slow drop in energy, a new headache, a change in appetite, or a sudden spike in anxiety. It’s about knowing when to adjust, when to wait, and when to switch. And it’s why the posts below cover everything from tamoxifen and SSRIs to how your expectations shape side effects, what happens when you switch generics, and why some combinations can be deadly. These aren’t just stories. They’re real-world checklists you can use to stay in control—without guessing.