Antidepressant Suicide Risk: What You Need to Know About the Warning and Real Data
When you start an antidepressant, a medication used to treat depression and some anxiety disorders by balancing brain chemicals. Also known as antidepressive agents, these drugs can change how you feel—but for a small group, they may temporarily increase thoughts of self-harm. This isn’t a myth. It’s a documented, FDA-mandated warning on most prescriptions. But here’s what most people miss: the risk isn’t about the drug being dangerous—it’s about the brain rewiring itself during early treatment.
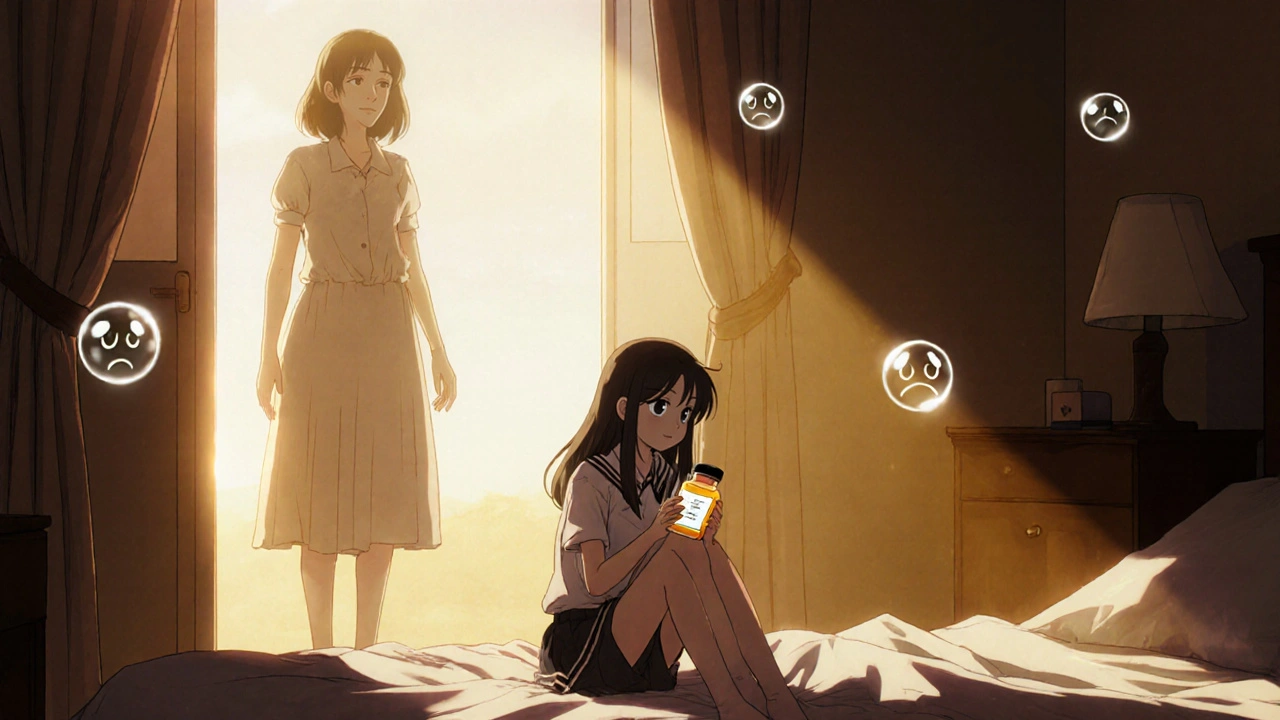
The highest risk isn’t for people with severe depression. It’s for younger adults, teens, and kids—especially in the first 1 to 4 weeks after starting a new SSRI, a class of antidepressants that increase serotonin levels, commonly prescribed for depression and anxiety. Also known as selective serotonin reuptake inhibitors, these include drugs like fluoxetine, sertraline, and escitalopram. Why? Because as energy returns before mood improves, someone might gain the physical ability to act on thoughts they previously lacked the strength to act on. This is why doctors monitor closely in the first month. It’s not because the drug causes suicide—it’s because it can give someone the push to act on existing thoughts.
What about older adults? The risk drops sharply after age 25. In fact, for people over 65, antidepressants lower suicide risk overall. The data shows that over time, these medications save lives. The warning exists because we’ve seen rare but tragic cases in younger patients—cases that could often be prevented with proper follow-up, not by avoiding treatment altogether.
And it’s not just about the drug. The medication safety, the practice of ensuring drugs are used correctly to minimize harm and maximize benefit. Also known as drug safety, it includes monitoring side effects, checking for interactions, and adjusting doses as needed. matters just as much as the prescription itself. Mixing antidepressants with alcohol, certain painkillers, or even herbal supplements like St. John’s Wort can raise the risk of dangerous reactions. And if you’ve ever switched brands or generics, you’ve probably noticed how even small changes in how a pill looks can trigger anxiety—sometimes leading to perceived side effects that aren’t even from the drug.
So what should you do? If you’re starting an antidepressant, know that the first few weeks are the most critical—not because the drug is toxic, but because your brain is adjusting. Talk to your doctor about warning signs: increased agitation, panic attacks, insomnia, or sudden shifts in mood. Keep your support system informed. Don’t stop suddenly. And if you feel worse, call your provider—don’t wait for your next appointment.
The truth is, most people who take antidepressants don’t have suicidal thoughts. But for those who do, the right support and monitoring can make all the difference. Below, you’ll find real stories and studies that cut through the noise—showing exactly when the risk is real, when it’s exaggerated, and how to navigate treatment safely.