Antidepressants and Youth Risk: What Parents and Teens Need to Know
When antidepressants, medications used to treat depression and anxiety by balancing brain chemicals are prescribed to teens, the goal is relief—not risk. But the reality is more complicated. While these drugs can lift mood and restore function, studies show a small but real increase in suicidal thoughts and behaviors in some young people during the first few weeks of treatment. This isn’t a reason to avoid treatment, but it is a reason to be informed. The SSRI side effects, a class of antidepressants including fluoxetine and sertraline that affect serotonin levels are the most commonly prescribed for teens, yet they’re not risk-free. What matters most isn’t just the drug, but how it’s started, monitored, and supported.
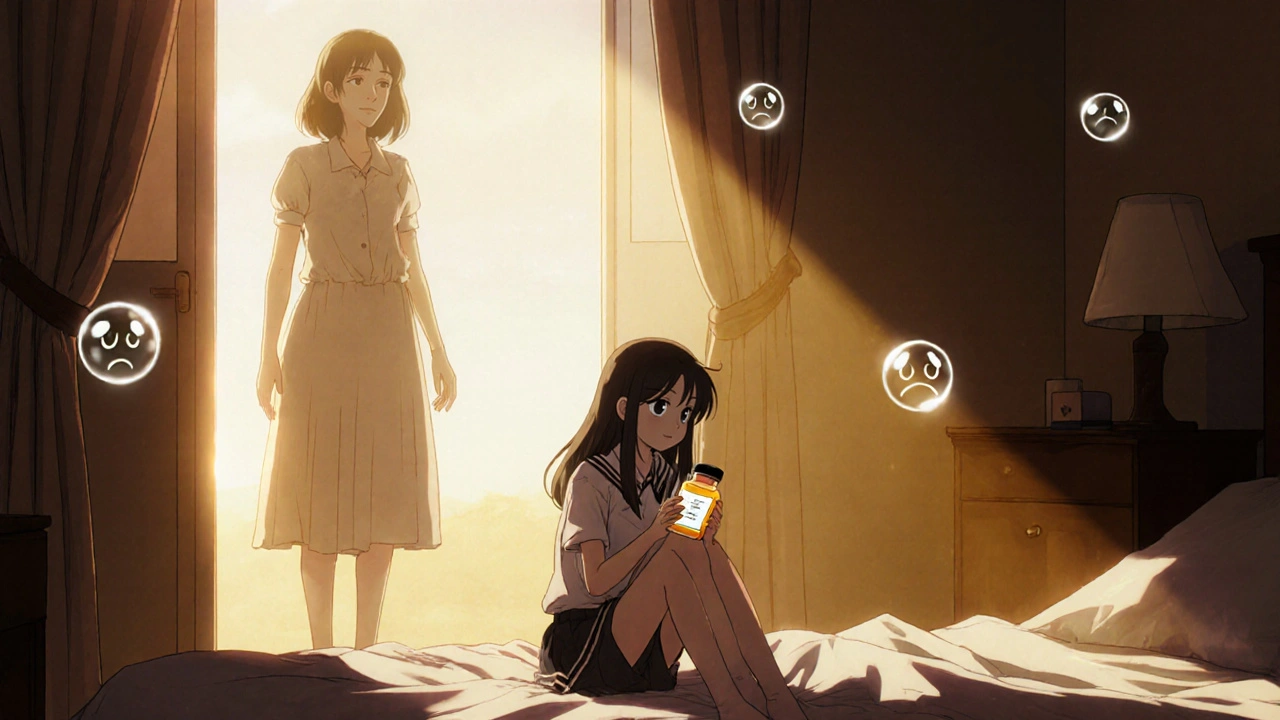
Parents often worry about changes in behavior: increased agitation, sleeplessness, or withdrawal. These aren’t always signs of worsening depression—they can be early reactions to the medication itself. The teen depression treatment, a structured approach combining therapy, medication, and family support for adolescents that works best doesn’t rely on pills alone. Therapy, especially CBT, is often the first step. When meds are added, close follow-up in the first 4–8 weeks makes all the difference. The FDA requires black box warnings on antidepressants for youth because the risk, while small, is real and measurable. But ignoring depression is far riskier. Untreated depression in teens leads to school failure, substance use, self-harm, and even suicide. The key is balance: not avoiding medication, but using it wisely.
Not all antidepressants carry the same level of risk. Fluoxetine (Prozac) is the only one with strong evidence supporting its safety and effectiveness in teens, which is why it’s often the first choice. Others, like paroxetine, have more troubling data in younger populations. It’s also important to know that medication safety, the practice of using drugs in a way that minimizes harm and maximizes benefit isn’t just about picking the right pill—it’s about knowing what else the teen is taking. Over-the-counter supplements, alcohol, even certain cough medicines can interact dangerously. And the antidepressant interactions, when two or more drugs affect each other’s function, potentially increasing side effects or reducing effectiveness with other prescriptions aren’t always obvious. That’s why regular check-ins with the prescribing doctor aren’t optional—they’re essential.
What you’ll find in the posts below isn’t theory. It’s real-world insight from studies and clinical experience. You’ll see how drug interactions can quietly undermine treatment, why placebo effects shape how teens feel on meds, and how generational attitudes toward pills affect outcomes. Some posts dig into the science behind why certain antidepressants are safer than others. Others show how expectations, brand perception, and even the wording on a prescription bottle can change how a teen responds. This isn’t about scare tactics. It’s about giving you the facts you need to make smart, calm decisions—for your teen, and for yourself.