Inflammation: Understanding the Body’s Alarm System
When dealing with inflammation, the body's natural defensive response that shows up as redness, heat, swelling, and pain. Also known as the inflammatory process, it kicks in when immune cells release cytokines to protect tissue. A popular way to calm skin inflammation is cryotherapy, the controlled application of cold to shrink blood vessels and blunt painful signals, while azelaic acid, a naturally occurring dicarboxylic acid that limits keratin buildup and modulates inflammation is favored for oily and acne‑prone skin. Another common anti‑inflammatory tool is fluticasone nasal spray, a corticosteroid that reduces swelling in the nasal passages. Together these approaches illustrate how both physical and pharmacologic methods target the same biological pathway.
Why Understanding Inflammation Matters
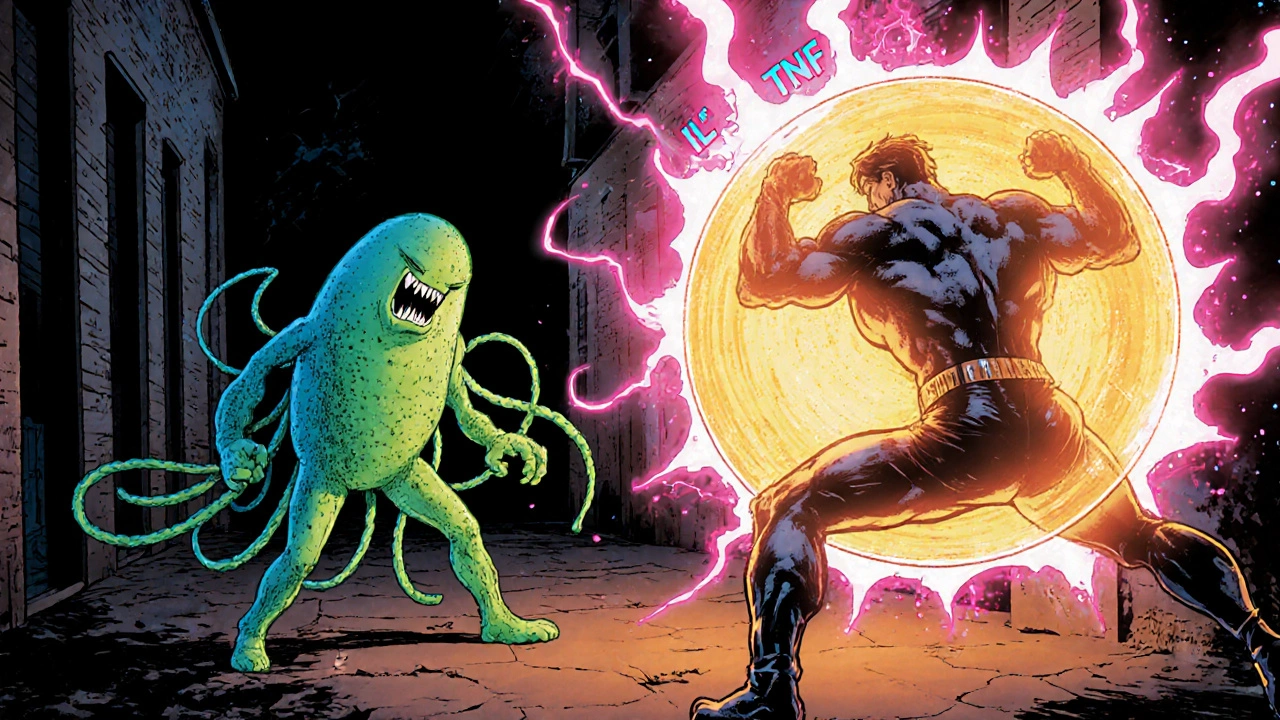
Inflammation isn’t just a skin issue; it’s a systemic signal that can drive chronic conditions. When cytokines like IL‑6 and TNF‑α stay elevated, they can impair insulin sensitivity, push blood vessels toward atherosclerosis, and even accelerate lung tissue damage seen in emphysema. That’s why many of the articles below link inflammation to diabetes risk, respiratory disease, and cancer‑related muscle weakness. Recognizing the link helps you spot early red flags and choose interventions that hit the root cause rather than just the symptoms.
Medications can tip the balance, too. Antivirals such as acyclovir may stress the kidneys and indirectly heighten inflammatory stress if combined with nephrotoxic drugs. Antibiotics like cefuroxime, while fighting infection, can also modulate the immune response—sometimes suppressing harmful inflammation, other times triggering a rebound effect. Knowing these interaction patterns lets you work with your clinician to keep inflammation from spiraling when you start a new prescription.
Lifestyle choices are powerful levers. Caffeine, for instance, can spark muscle spasms in people prone to electrolyte shifts, which in turn fuels local inflammation. Hormone replacement therapy during menopause may either dampen or aggravate vaginal and systemic inflammation depending on the formulation. Simple tweaks—hydrating, balanced meals rich in omega‑3 fatty acids, and regular low‑impact exercise—can lower baseline cytokine levels and make your body less reactive to triggers.
Emerging therapies push the envelope further. The experimental “Advanced D” drug aims to curb age‑related inflammation by targeting senescent cell pathways, while new lithium‑based battery research hints at high‑energy delivery for medical devices that could improve inflammation monitoring. Even mental‑health solutions like Algikey show that reducing stress hormones can indirectly calm inflammatory cascades.
All of these angles—cold therapy, topical acids, inhaled steroids, drug‑interaction awareness, nutrition, and cutting‑edge research—form a web where each strand supports the others. By weaving them together you get a flexible, personalized plan that addresses inflammation wherever it shows up.
Below you’ll find a curated set of articles that dig into each of these topics in detail. Whether you’re looking for safe ways to combine medications, practical tips to soothe skin flare‑ups, or the latest science on anti‑aging inflammation control, the collection offers clear, actionable guidance ready to help you manage inflammation effectively.