Prevent Anesthesia Risks: A Practical Guide
When talking about preventing anesthesia risks, the goal is to keep patients safe before, during, and after surgery by spotting hazards early and managing them effectively. Also known as anesthesia safety, it covers everything from drug choices to monitoring equipment. Prevent anesthesia risks starts with a solid plan, not a last‑minute scramble.
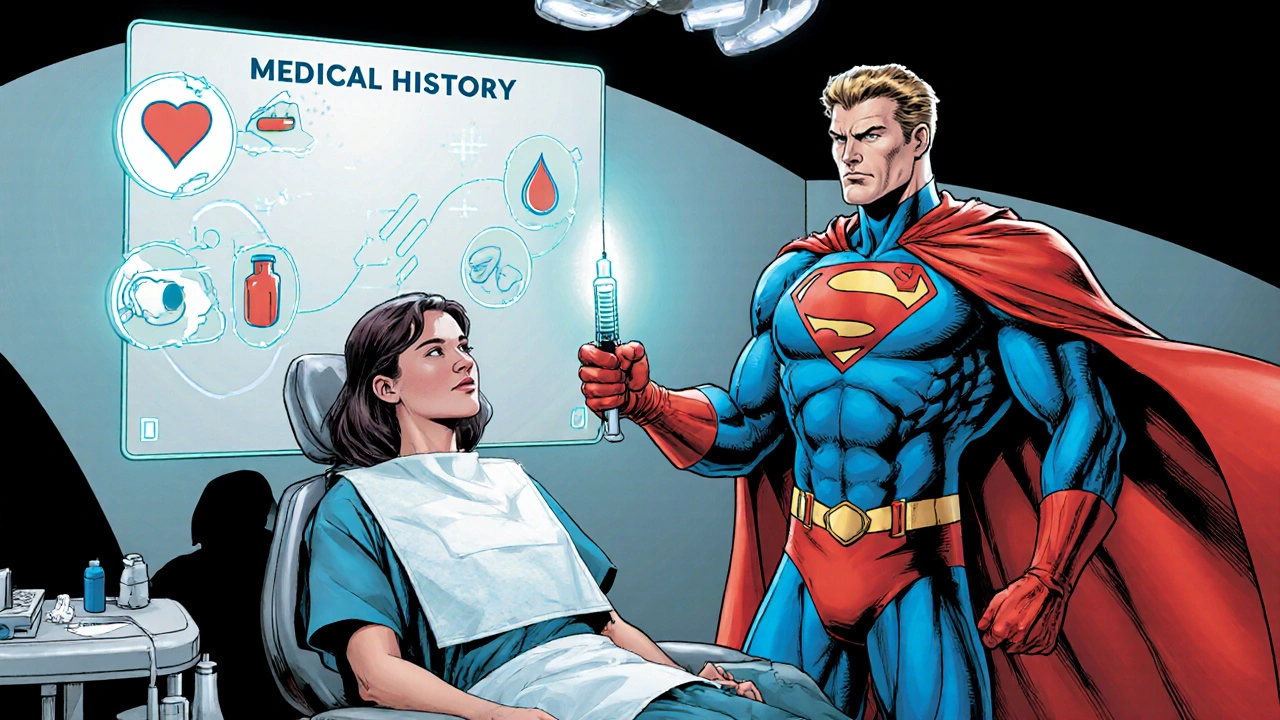
Why a solid preoperative assessment matters
Your first line of defense is a thorough preoperative assessment, a systematic review of the patient’s health, meds, allergies and lab results before any anesthetic is given. This step uncovers hidden conditions like sleep apnea or heart disease that could turn a routine case into an emergency. By documenting these factors, the anesthesiologist can tailor drug doses and choose suitable techniques, cutting the chance of unexpected reactions. In short, preoperative assessment encompasses risk identification and mitigation.
When the assessment is done right, the next big factor is drug safety. Many patients are already on multiple prescriptions, over‑the‑counter meds or supplements. That’s where drug interactions, the ways in which one medication can alter the effect or metabolism of another, become critical for anesthesia planning. For example, certain antidepressants can boost the potency of muscle relaxants, while NSAIDs might increase bleeding risk when combined with regional blocks. Knowing these links ahead of time lets the team adjust doses or swap drugs, which influences anesthesia safety directly.
Even with perfect assessments and cleared meds, the operating room is a dynamic environment. Continuous patient monitoring, real‑time tracking of vital signs, oxygen levels, and anesthesia depth throughout the procedure acts as the safety net that catches problems the moment they arise. Modern monitors alert staff to changes in blood pressure, heart rhythm or oxygen saturation within seconds, allowing rapid intervention. This proactive oversight reduces complications like hypoxia or hemodynamic instability, making monitoring a cornerstone of risk prevention.
Choosing the right anesthetic agents is another layer that supports the safety net. Short‑acting inhalational gases and ultra‑short opioids give the anesthesiologist fine‑tuned control, especially for patients with comorbidities uncovered during assessment. When agents are matched to the patient’s physiology, recovery times shorten and side‑effects drop, directly supporting the goal of keeping risks low.
All these pieces—assessment, drug interaction checks, monitoring, and agent selection—work best when the surgical team communicates clearly. A brief, structured handoff between surgeon, anesthesiologist, and nursing staff ensures everyone knows the patient’s risk profile and the plan to manage it. This teamwork enables rapid decision‑making if something unexpected happens, tightening the safety loop.
Below you’ll find a curated collection of articles that dive deeper into each of these areas. Whether you’re looking for tips on medication safety, monitoring technology, or pre‑op checklists, the posts ahead give practical, evidence‑based advice you can apply right away.